News
Featured Articles
Stop by AGA Central during DDW®
See the 11 mentors voted best in our field
Discover inspiring research at DDW® 2024
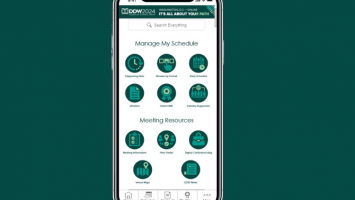
Just launched: DDW® 2024 Mobile App
Three weeks left to register for DDW®
How to navigate mentorship
Review your reported provider data in Open Payments
The Shark Tank winner is Arithmedics!
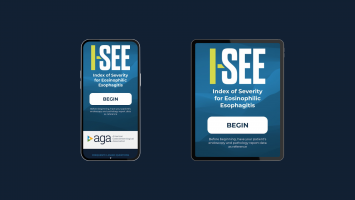
Have you downloaded the I-SEE mobile app yet?
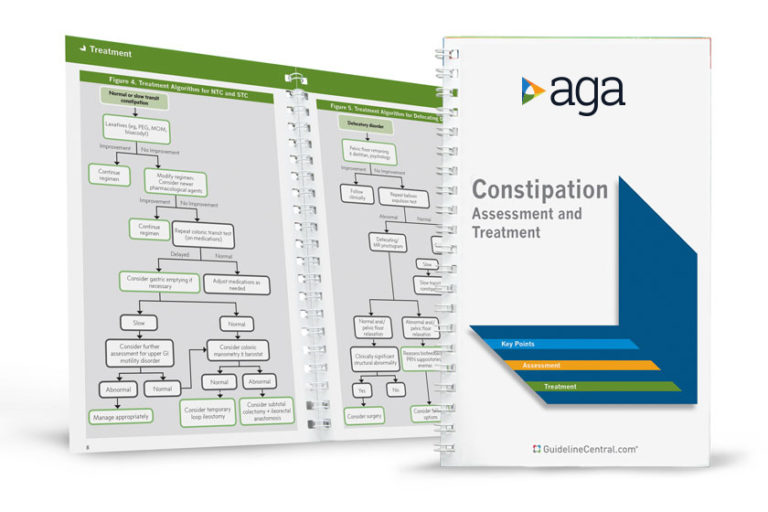
AGA Pocket Guides
Official AGA Institute quick-reference tools provide healthcare providers and students with instant access to current guidelines and clinical care pathways in a clear, concise format. AGA Institute pocket guides are available in print and digital form.
Member Non-Member
AGA clinical guidance
Find the latest evidence-based recommendations for treating your patients.