News
Featured Articles
Congratulations to the 2024 AGA Research Foundation awardees!
An inspiring weekend in LA with women in GI
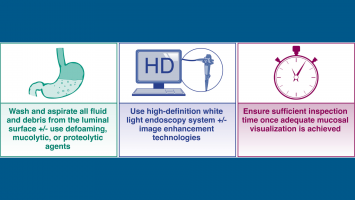
Nine tips to improve your upper endoscopy exams
Introducing your 2024 AGA recognition prize recipients
Get an inside look at cannabinoid hyperemesis syndrome in our latest clinical practice update
Stop by AGA Central during DDW®
See the 11 mentors voted best in our field
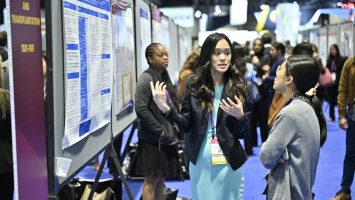
Discover inspiring research at DDW® 2024
Just launched: DDW® 2024 Mobile App
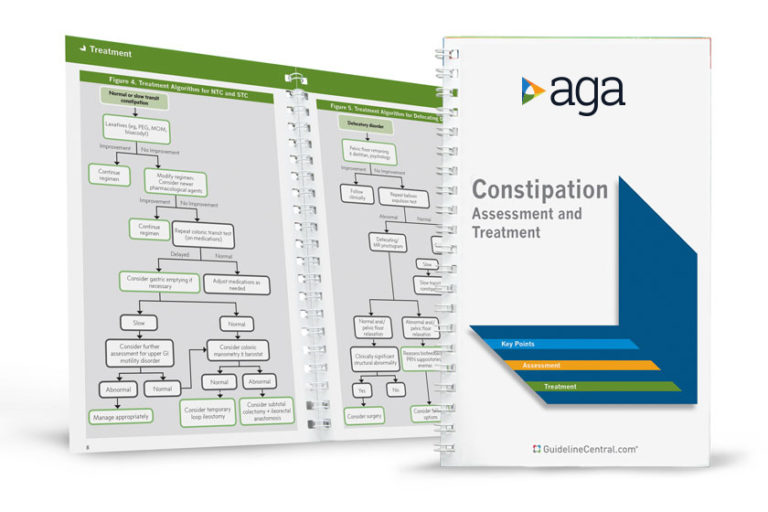
AGA Pocket Guides
Official AGA Institute quick-reference tools provide healthcare providers and students with instant access to current guidelines and clinical care pathways in a clear, concise format. AGA Institute pocket guides are available in print and digital form.
Member Non-Member
AGA clinical guidance
Find the latest evidence-based recommendations for treating your patients.