News
Featured Articles
Stop by AGA Central during DDW®
See the 11 mentors voted best in our field
Discover inspiring research at DDW® 2024
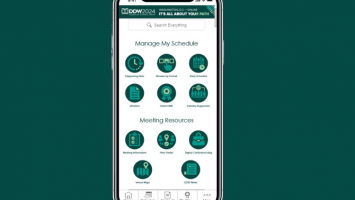
Just launched: DDW® 2024 Mobile App
Three weeks left to register for DDW®
Join AGA for international education opportunities at DDW 2024
How to navigate mentorship
Review your reported provider data in Open Payments
The Shark Tank winner is Arithmedics!
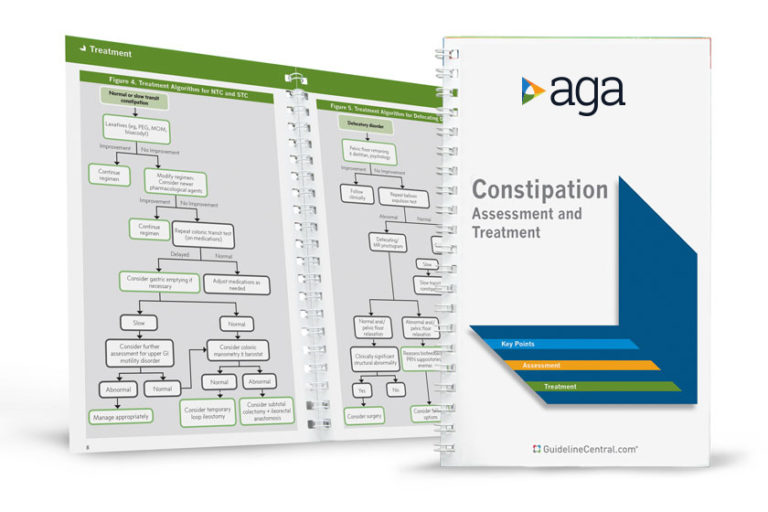
AGA Pocket Guides
Official AGA Institute quick-reference tools provide healthcare providers and students with instant access to current guidelines and clinical care pathways in a clear, concise format. AGA Institute pocket guides are available in print and digital form.
Member Non-Member
AGA clinical guidance
Find the latest evidence-based recommendations for treating your patients.