Home > Advocacy & Policy > Policies Affecting GI > Physician Reimbursement and Quality Payment Program Reform
Physician Reimbursement and Quality Payment Program Reform
In its current form, the QPP has posed significant challenges to physicians. We ask Congress to reform QPP and stabilize Medicare reimbursement.
AGA position: Congress must enact reforms to the Quality Payment Program (QPP) to ensure the program is clinically relevant to all physicians and their patients and provides stable reimbursement for physicians who care for Medicare patients.
The Medicare Access and CHIP Reauthorization Act (MACRA) was signed into law in April 2015, and replaced the flawed sustainable growth rate (SGR) formula with the Quality Payment Program (QPP). The QPP is comprised of two tracks: the Merit-based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (Advanced APMs). The Centers for Medicare & Medicaid Services (CMS) began implementing the QPP on Jan. 1, 2017 with the goal of moving providers out of MIPS and into Advanced APMs. To accomplish this, Congress expanded the scope of the Physician Focused Payment Model Technical Advisory Committee (PTAC) to provide feedback and technical assistance on alternative payment models.
The QPP falls short
In its current form, the QPP has posed significant challenges to physicians. Specialists, in particular, have struggled to meaningfully participate in MIPS or engage in alternative APMs. Despite the expanded scope of PTAC’s work, CMS has failed to pilot or implement several specialty alternative payment and delivery models including ones for gastroenterologists. Additionally, the statutory reimbursement updates have failed to keep pace with rising inflation, leading to inadequate reimbursement for physicians’ services.
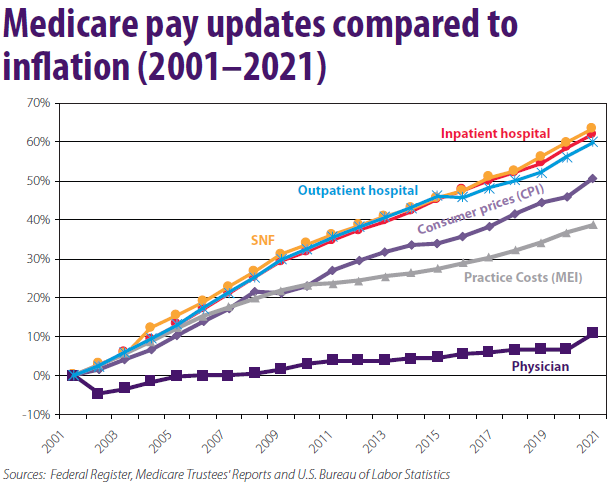
According to an American Medical Association (AMA) analysis of the Medicare Trustees data, the cost of running a medical practice increased 39 percent between 2001 and 2021, while inflation-adjusted Medicare physician reimbursements declined 20 percent during that same period (see figure below).
Flaws in QPP administration
CMS has created disjointed, administratively burdensome, and clinically irrelevant pathways under the MIPS program, which:
- Disincentivizes the use of specialty-specific quality measures that are meaningful to patients and clinicians
- Results in unnecessary and duplicative reporting
- Fails to create a glide path to prepare specialists to move into APMs
- Does little to improve patient care and outcomes.
An October 2021 report issued by the U.S. Government Accountability Office (GAO) expressed concern that MIPS performance feedback is neither timely nor meaningful, questioned whether the program helps improve quality and patient outcomes, and highlighted the program’s low return on investment.
Few specialty-specific payment models
Thus far, the Department of Health and Human Services has yet to implement any of the options recommended by PTAC. This not only discourages the development of more innovative models but significantly limits the movement of specialists into value-based models. Without the inclusion of specialty models, payment reform is likely to be unsuccessful, entrench current problems in QPP, and will exclude the highest cost, most complicated patients.
AGA asks Congress to:
- Enact meaningful reforms to the QPP that recognize the value of specialty care and provides payment stability for physicians.
- Provide effective oversight of the QPP to determine its effectiveness at measuring performance and outcomes.
- Stabilize Medicare physician reimbursements while exploring more permanent solutions.
- Provide ongoing, temporary relief from physician payment cuts caused by PayGo, sequestration, and budget neutrality adjustments to the conversion factor and disruptions due to the COVID-19 pandemic.
Reviewed: February 2022










