AGA’s newest Clinical Practice Update provides an expert review on the evaluation and management of belching, abdominal bloating and distention.
These symptoms are common complaints for patients seeking outpatient gastroenterology consults.
Belching
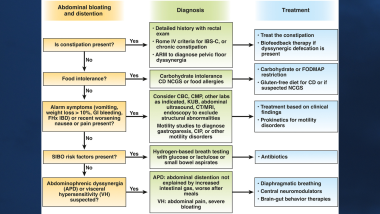
Rome IV defines belching as an audible escape of air from the esophagus or the stomach into the pharynx. Belching is subdivided into supragastric belching from the esophagus and gastric belching from the stomach.
Belching is different from aerophagia where excessive swallowing of air increases intragastric and intestinal gas which leads to bloating, distention and flatulence.
High-resolution esophageal manometry, if combined with impedance monitoring (with and without pH) can help differentiate gastric and supragastric belching and aerophagia.
A biopsychosocial history should also be taken to address factors like anxiety, life events and conditioned responses to the stressors of physical symptoms.
Brain-gut behavioral therapies are the most effective treatment for patients with supragastric belching. Examples include: diaphragmatic breathing, cognitive behavioral therapy, relaxation training and gut-directed hypnotherapy. Central neuromodulators can also improve symptom burden and quality of life.
Use the below algorithm to set the diagnosis and management plan for supragastric belching, gastric belching and aerophagia.
Abdominal bloating and distention
Abdominal bloating is a subjective sensation experienced by patients as fullness, swelling, trapped gas or tightness. Abdominal distention is a visible increase in abdominal girth.
The Rome IV criteria define functional bloating and distention as DGBIs with recurrent symptoms of abdominal fullness or pressure or a visible increase in abdominal girth with symptoms at least 1 day per week for 3 months. Patients should not have have a co-morbid diagnosis of IBS, functional constipation, functional diarrhea or functional dyspepsia.
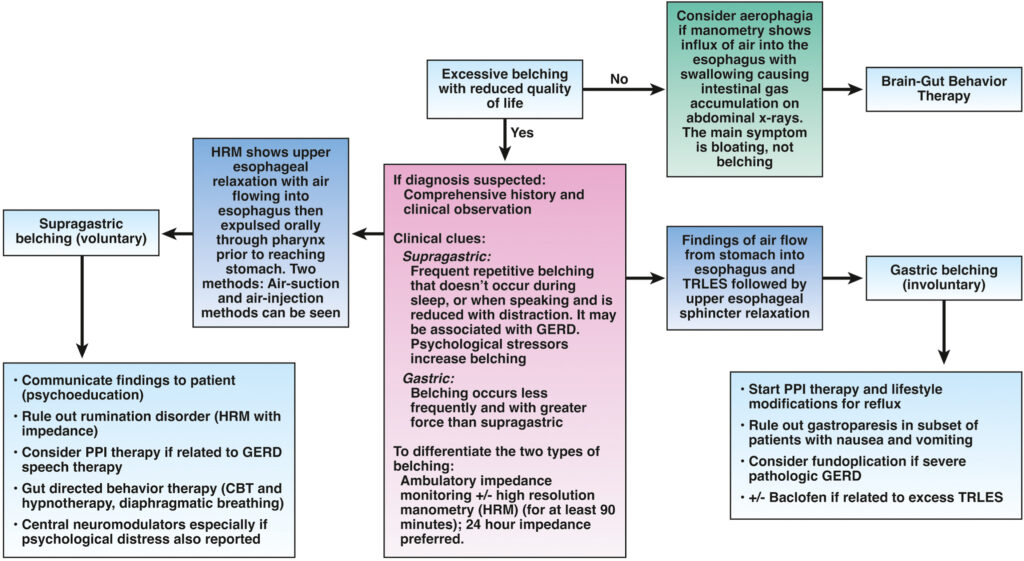
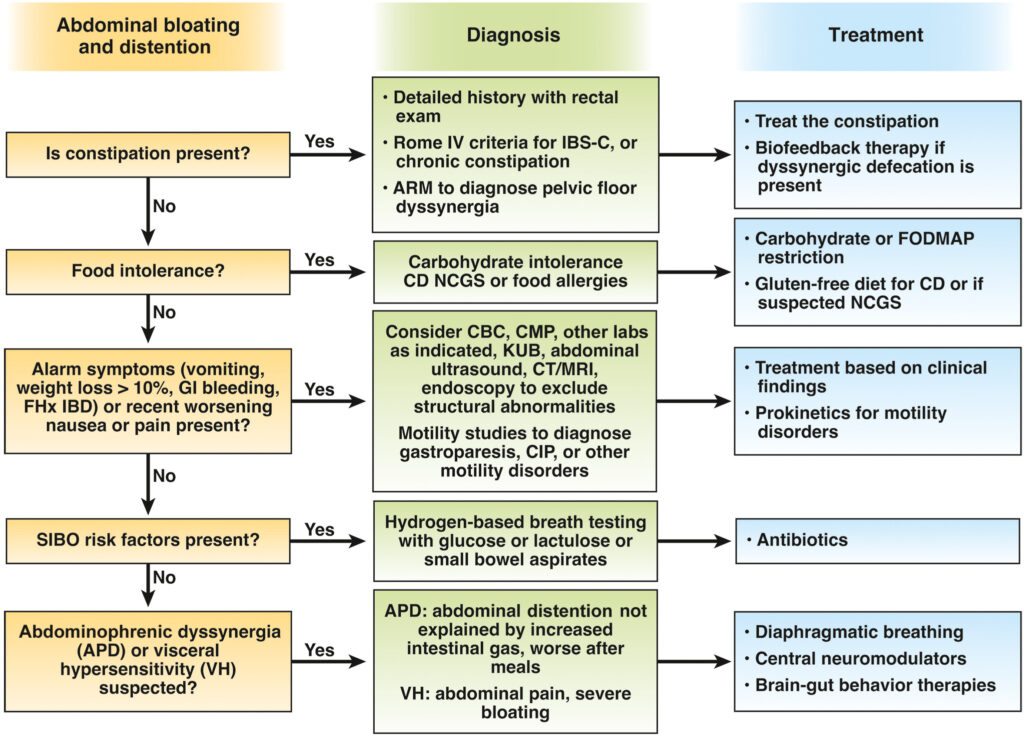
Diagnostic testing will depend on an algorithmic approach based on presumptive causes as shown below.
- Food intolerances or hypersensitivity such as lactose or fructose intolerance and nonceliac gluten sensitivity
- SIBO
- Celiac disease
- Motility disorders
There is a lack of scientific evidence for successful treatments for abdominal bloating and distention.
In patients with DGBI, effective communication is key to educating patients on brain-gut interactions so that treatments such as diet, biofeedback therapy, central neuromodulators and psychotherapies can be trialed.
Probiotics are not recommended for the treatment of bloating or distention.
The authors gave 15 best practice advice statements for addressing these symptoms in patients, while also concluding that both a multidisciplinary and patient-centered approach are key to treating patients with disorders of gut-brain interaction.
Quick watch:
Author Dr. Baha Moshiree explains supragastric vs. gastric belching and overlap syndromes in regard to bloating and distention.
Read the full AGA Clinical Practice Update on Evaluation and Management of Belching, Abdominal Bloating, and Distention: Expert Review, published in the September issue of Gastroenterology.