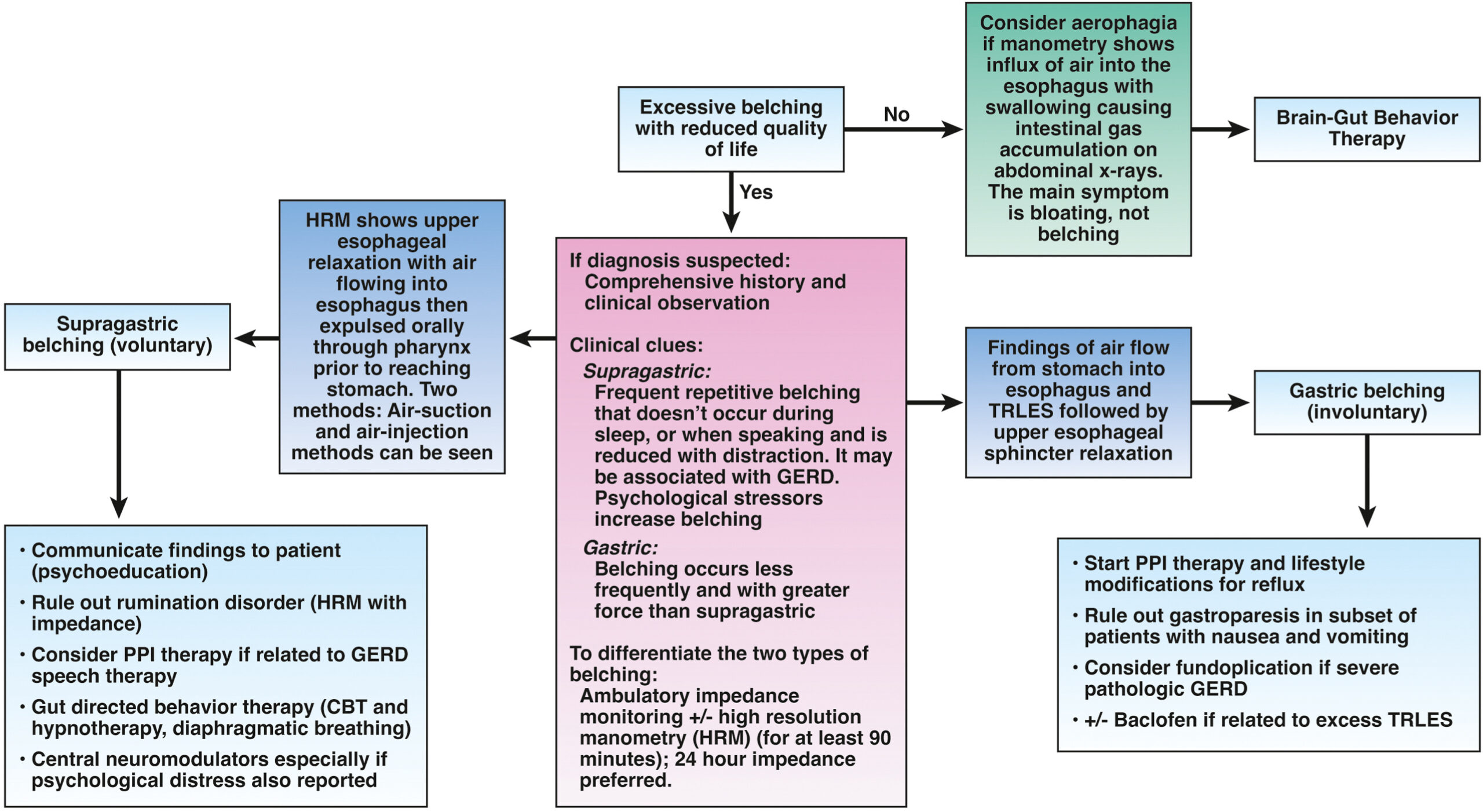
1. Clinical history and physical examination findings and impedance pH monitoring can help to differentiate between gastric and supragastric belching.
2. Treatment options for supragastric belching may include brain-gut behavioral therapies, either separately or in combination, such as cognitive behavioral therapy, diaphragmatic breathing, speech therapy and central neuromodulators.
3. Rome IV criteria should be used to diagnose primary abdominal bloating and distention.
4. Carbohydrate enzyme deficiencies may be ruled out with dietary restriction and/or breath testing. In a small subset of at-risk patients, small bowel aspiration and glucose- or lactulose-based hydrogen breath testing may be used to evaluate for small intestinal bacterial overgrowth.
5. Serologic testing may rule out celiac disease in patients with bloating and, if serologies are positive, a small bowel biopsy should be done to confirm the diagnosis. A gastroenterology dietitian should be part of the multidisciplinary approach to care for patients with celiac disease and nonceliac gluten sensitivity.
6. Abdominal imaging and upper endoscopy should be ordered in patients with alarm features, recent worsening symptoms, or an abnormal physical examination only.
7. Gastric emptying studies should not be ordered routinely for bloating and distention, but may be considered if nausea and vomiting are present. Whole gut motility and radiopaque transit studies should not be ordered unless other additional and treatment-refractory lower gastrointestinal symptoms exist to warrant testing for neuromyopathic disorders.
8. In patients with abdominal bloating and distention thought to be related to constipation or difficult evacuation, anorectal physiology testing is suggested to rule out a pelvic floor disorder.
9. When dietary modifications are needed (e.g., low-fermentable oligosaccharides, disaccharides, monosaccharides and polyols diet), a gastroenterology dietitian should preferably monitor treatment.
10. Probiotics should not be used to treat abdominal bloating and distention.
11. Biofeedback therapy may be effective for bloating and distention when a pelvic floor disorder is identified.
12. Central neuromodulators (e.g., antidepressants) are used to treat bloating and abdominal distention by reducing visceral hypersensitivity, raising sensation threshold and improving psychological comorbidities.
13. Medications used to treat constipation should be considered for treating bloating if constipation symptoms are present.
14. Psychological therapies, such as hypnotherapy, cognitive behavioral therapy and other brain-gut behavior therapies may be used to treat patients with bloating and distention.
15. Diaphragmatic breathing and central neuromodulators are used to treat abdominophrenic dyssynergia.