AGA leaders continue to raise concerns about UnitedHealthcare’s (UHC) failure to operate in good faith with its Advance Notification Program (ANP), and how the program is a precursor to additional red tape that will ultimately delay and disrupt care for patients who require colonoscopies and endoscopies.
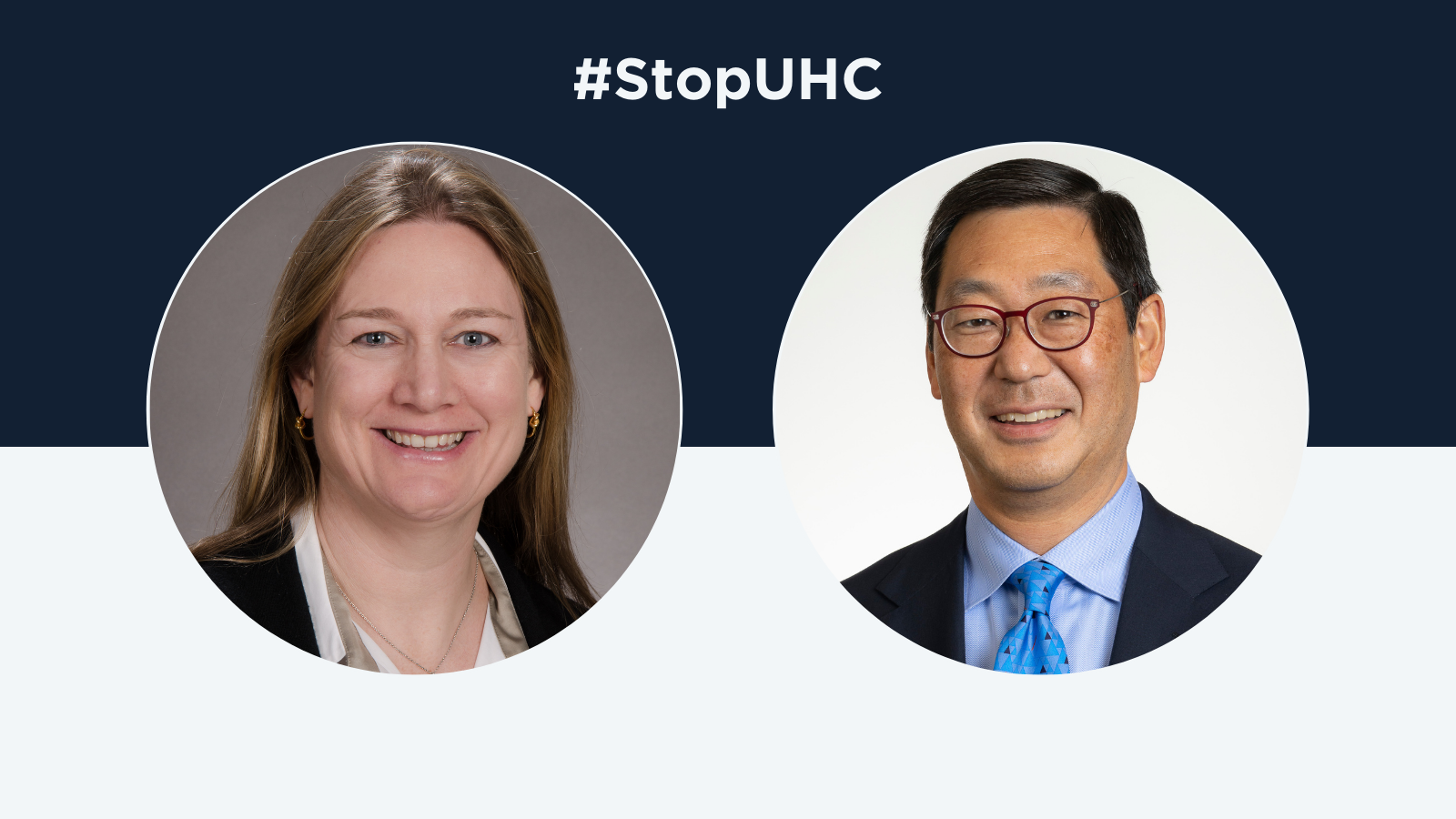
When UHC implemented ANP at the eleventh hour instead of its original prior authorization plan for GI and endoscopic procedures, “it really was a bait and switch,” AGA President Barbara Jung said in an interview with Modern Healthcare.
ANP is not a victory – it is “an amorphous data reporting policy for GI doctors that is already creating confusion and wasting precious time for office staff who should be performing more important duties – such as streamlining patient care,” AGA Vice President Larry Kim wrote in an editorial published on the Alliance of Specialty Medicine’s Medium channel.
While UHC claims data collection through ANP is required to inform whether colonoscopies and endoscopies are overutilized, it’s doubtful the insurer will get this data through this burdensome policy.
“Data show these vital services are actually underutilized,” Dr. Kim writes, noting that the program is instead “a last-ditch effort to find a rationale that justifies UHC’s “Gold Card” program that will go into effect early next year.”
Recent news coverage by Becker’s further emphasizes how the insurer has been uncommunicative since Dr. Jung’s letter in August. Additionally, UHC is facing mounting congressional pressure related to its consolidation practices as well.
Patients don’t need more barriers to care. We continue to call on UHC to work with the GI community to find a solution.