Electronic Gastro Curbside Consult
A 51-year-old man with past medical history of hypertension and alcohol use was initially admitted to an outside hospital for hematemesis. He underwent an upper endoscopy that revealed gastric varices that were banded. Imaging was performed and reportedly found splenic and portal vein thrombosis. He was started on Coumadin and subsequently discharged. He presented 5 days later with 5 episodes of hematemesis, each containing about 400 mL of bright red blood. The patient underwent transfusion of 5 U of packed red blood cells and fresh frozen plasma and was airlifted to our hospital. En route the patient had another episode of emesis vomiting 500 mL of blood.
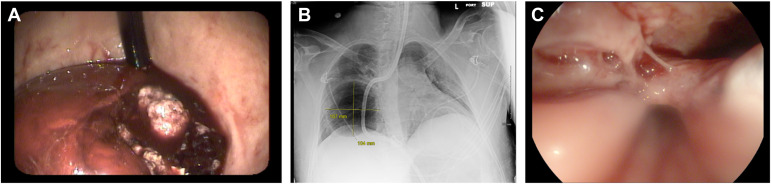
Computed tomography (CT) showed evidence of gastric varices and splenic vein thrombosis. An emergent upper endoscopy showed no evidence of esophageal varices. The stomach showed a large amount of fresh blood mixed with clot and, despite suctioning for 45 min with a therapeutic scope, there was inadequate visualization of the proximal stomach and fundus (Figure A).
Given active bleeding on endoscopy and unstable vitals, a decision was made to place a Blakemore tube (BT) to tamponade the bleeding under direct visualization with the endoscope. Subsequently 50 mL of air was placed in the gastric balloon. Postinflation chest X-ray verified position of gastric balloon in stomach. After confirmation, the gastric balloon was inflated with 250 mL of air. The balloon was pulled to the gastroesophageal junction and traction was placed with pulley system with a 1-lb weight. Subsequently a repeat chest X-ray post procedure was performed (Figures B, C).
What is your diagnosis and next intervention?
To find out the diagnosis, review treatment options and hear the patient outcome, review the full case published in Gastroenterology.












