Clinical Gastroenterology and Hepatology image of the month:
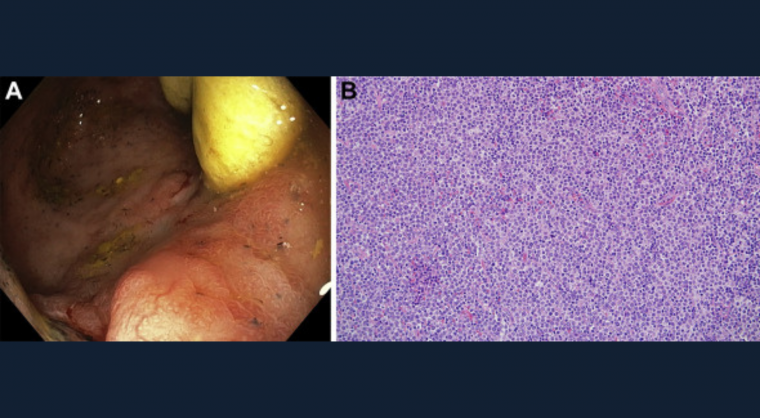
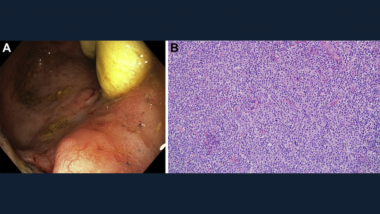
A 61-year-old woman with a diagnosis of left-sided ulcerative colitis presented with recurrence of watery nonbloody diarrhea. She was status post liver transplant 2 years prior for primary sclerosing cholangitis, currently on tacrolimus and mesalamine. Following a negative Clostridium difficile polymerase chain reaction, colonoscopy demonstrated Mayo 1 appearance throughout the colon, with an area of friable and hemorrhagic mucosa in the cecum (Figure A). Random colon biopsies showed mild chronic active colitis, but specific biopsies of the cecal patch identified a monomorphous infiltrate of atypical lymphocytes (Figure B). Immunohistochemistry confirmed CD20 and Epstein-Barr virus–positive lymphocytes (Figure C), supporting the diagnosis of post-transplant lymphoproliferative disorder (PTLD). Positron emission tomography scan confirmed the malignancy was restricted to the cecum (Figure D, arrow).
Although PTLD is a well-identified complication of solid organ transplant, PTLD isolated to the colon is rare. Immunosuppressive therapy is the major risk factor, and although drug withdrawal can be therapeutic, it should be balanced with the risk of organ rejection. Tacrolimus dose was reduced from 3 mg twice daily to 1 mg twice daily and the patient opted for partial ileocecectomy with temporary diverting ileostomy, with follow-up scheduled 6-months postoperatively. PTLD is an important complication of transplant immunosuppression that should be particularly considered in the management of primary sclerosing cholangitis inflammatory bowel disease patients post liver transplant.
View this case in the latest issue of Clinical Gastroenterology and Hepatology.