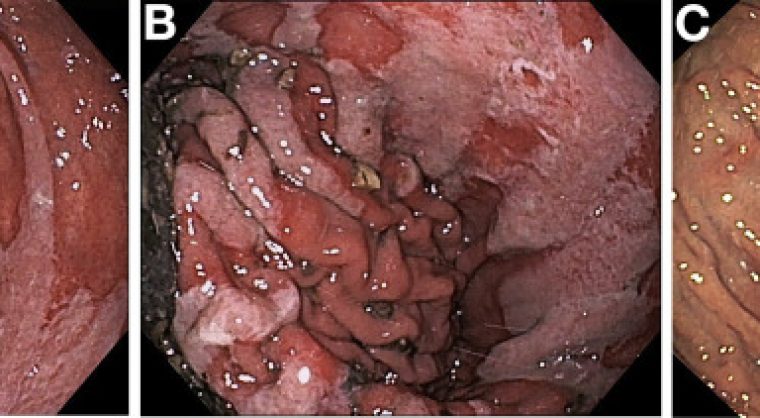
Clinical Gastroenterology and Hepatology (CGH) Image of the Month: An 81-year-old woman presented with coffee-ground emesis, with no other symptoms associated. The patient had history of atrial fibrillation and symptomatic polyarticular arthropathy. She was medicated with rivaroxaban, naproxen and pantoprazole 20 mg. Physical examination was unremarkable, and she was hemodynamically stable. Laboratory evaluation revealed normocytic anemia (10.3 g/dL). The patient underwent upper gastrointestinal endoscopy, which showed a large hiatal hernia (about 9 cm long) with digested food and blood in its sac (figure A). Along the diaphragmatic impression, a set of contiguous clean-based linear ulcers and erosions was observed, consistent with Cameron lesions (figure B). No other sources of bleeding were found. Intravenous proton pump inhibitor was started, and naproxen was discontinued. She recovered uneventfully. Helicobacter pylori test was negative. Endoscopic follow-up 12 weeks later showed healing of the lesions (figure C). Hernia repair was discussed, but the patient refused any surgical intervention. She remains on proton pump inhibitor therapy without recurrence of bleeding or anemia.
This case highlights that Cameron lesions, although rare, can be a clinically significant cause of upper gastrointestinal bleeding. The patients are frequently elderly women with large hiatal hernias. Long-term acid suppression is the mainstay of treatment; surgical repair is reserved for refractory or complicated disease.
This image case was featured in the October issue of CGH.