Gastroenterology clinical image challenge: A 9-year-old boy presented with an episode of chest pain and recurrent fever. He had a prior history of Crohn’s disease with ileal and colonic involvement diagnosed at the age of six. Clinical remission was achieved under combination therapy including infliximab (5 mg/kg every eight weeks) and azathioprine. One year before this episode, he presented with back pain, fever and inflammatory syndrome (C-reactive protein of 120 mg/L) without any signs of Crohn’s disease relapse. A computed tomography (CT) scan showed a right lung infection with pleural effusion. Amoxicillin treatment was initiated with efficacy on pain, fever and the biological inflammation.
The current symptoms include severe back and chest pains with no efficacy of oral or local analgesic, fever, and inflammatory syndrome (C-reactive protein of 150 mg/L). There was no sign of Crohn’s disease activity at abdominal ultrasound. Echocardiography, electrocardiogram, chest radiograph and bone scintigraphy were normal.
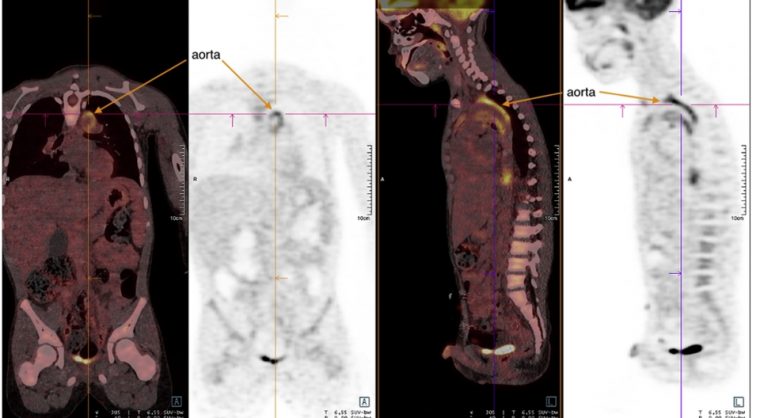
A body positron emission tomography (PET)–CT scan (figure) showed several foci of hypermetabolism located in the vascular wall of the aorta that could be evocative of an inflammatory disease. Magnetic resonance imaging of the aorta confirmed the presence of an aortitis with an extension to the subaortic trunk and showed a thickening of the vascular walls with hyperintense signals specific for inflammation (T2 and T1 post gadolinium). The narrowing of the abdominal aorta that was nonsignificant (less than 50%) on the CT scan.
Immune-inflammatory tests were unspecific (antinuclear antibody, 1/640; anti-DNA, 55 UI/mL; antiextractable nuclear antigens, negative; rheumatoid factor, negative; HLA B27, negative; angiotensin-converting enzyme, negative). Blood tests for infectious aortitis (syphilis, tuberculosis, bacteria and fungi) were negative.
Considering the patient’s medical history and evolution, what is the diagnosis?
To find out the diagnosis, read the full case in Gastroenterology.