Gastroenterology image challenge: A 79-year-old man presented to the hospital after several weeks of easy bruising and a syncopal episode. On admission he was noted to have a retroperitoneal hematoma requiring several transfusions. During initial evaluation his coagulation tests were noted to be abnormal, leading to the diagnosis of an acquired factor VIII inhibitor (FVIII; activity <1% and FVIII inhibitor level 408BU). He was treated with four doses of rituximab and high-dose steroids for several weeks with improvement in his FVIII activity level. He was admitted to our hospital several weeks later with a melena and fatigue. During this admission, he was noted to have new-onset pancytopenia (white blood cell count, 0.6K/μL; hemoglobin, 6.6 M/μL; platelets, 87K/μL). A broad workup for pancytopenia was initiated with normal vitamin B12, folate, and copper, and nondetectable hepatitis B and C virus, HIV, and Epstein–Barr virus. Cytomegalovirus (CMV) viral load was 213,508 IU/mL, for which he was started on IV ganciclovir.
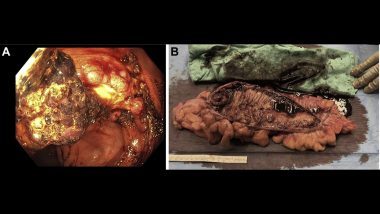
Melena persisted and was associated with hemodynamic instability requiring transfer to the intensive care unit. Esophagogastroduodenoscopy and colonoscopy were performed. Esophagogastroduodenoscopy demonstrated three small nonbleeding duodenal ulcers with no high-risk stigmata. Colonoscopy demonstrated a 5- to 6-cm fungating, ulcerated, nonobstructing mass in the ascending colon with active bleeding (figure A), which was firm on biopsy concerning for a malignancy. Colonic mass histology demonstrated ulcer with many CMV viral inclusions but no definitive evidence of malignancy. The patient continued to have ongoing bleeding with accompanying hemodynamic instability despite correction of underlying coagulopathy and initiation of antiviral therapy. Given ongoing colonic bleeding, lack of therapeutic endoscopic options, and concern for possible underlying malignancy, the decision was made to proceeded with surgical resection of the colonic mass (figure B).
What is most likely etiology of this colonic lesion?
To find out the diagnosis, read the full case in Gastroenterology.