-
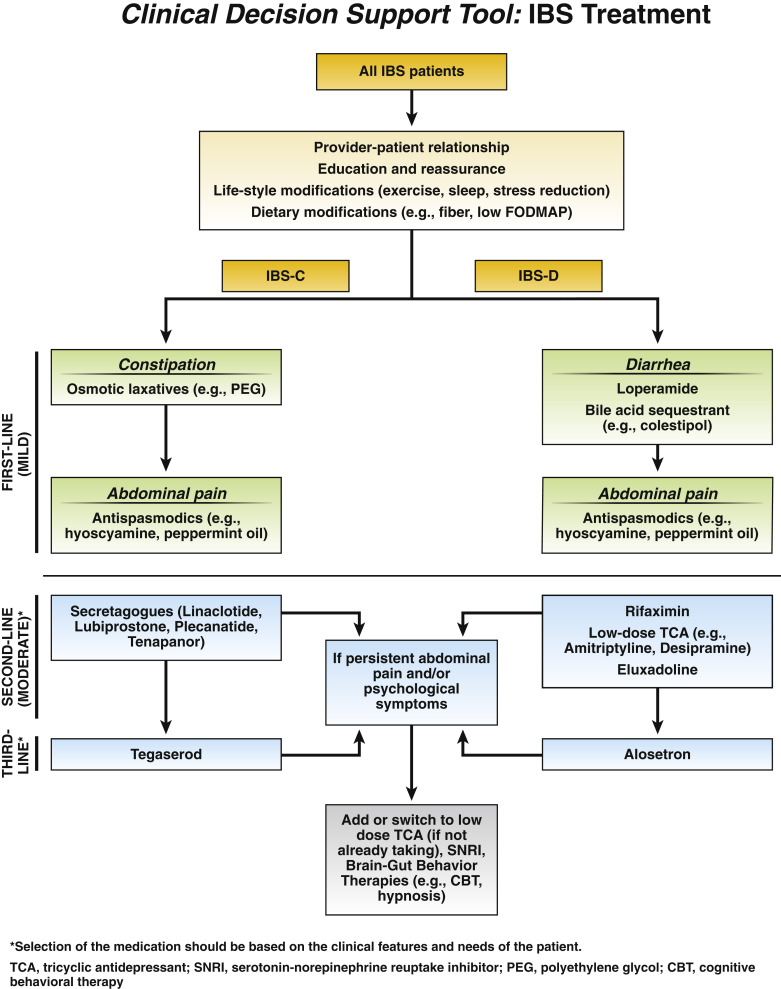
IBS-C pharmacologic recommendations
In patients with IBS-C, AGA suggests the use of tenapanor, plecanatide, tegaserod, lubiprostone and polyethylene glycol (PEG) laxatives.
In patients with IBS-C, AGA recommends using linaclotide.
Read the full clinical guidance.
-
IBS-D pharmacologic recommendations
In patients with IBS-D, AGA suggests the use of eluxadoline, alosetron and loperamide.
In patients with IBS-D, AGA suggests the use of rifaximin. In patients with an initial response to rifaximin who develop recurrent symptoms, AGA suggests retreatment with rifaximin.
Read the full clinical guidance.
-
General IBS recommendations
In patients with IBS, AGA suggests using tricyclic antidepressants (TCAs) and antispasmodics.
In patients with IBS, AGA suggests against using selective serotonin reuptake inhibitors (SSRIs).
-
Diet and IBS best practice advice
Diet advice is ideally prescribed to patients who have insight into their meal-related GI symptoms and are motivated to make the necessary changes. Referral to a registered dietitian nutritionist (RDN) should be made to patients who are willing to collaborate with an RDN and patients who are not able to implement beneficial dietary changes on their own.
Patients with IBS who are poor candidates for restrictive diet interventions include those consuming few culprit foods, those at risk for malnutrition, those who are food insecure, and those with an eating disorder or uncontrolled psychiatric disorder. Routine screening for disordered eating or eating disorders by careful dietary history is critical because they are common and often overlooked in GI conditions.
Patients should attempt specific IBS diet interventions for a predetermined length of time. If the patient has no clinical response, the diet intervention should be abandoned for another treatment alternative.
Soluble fiber is efficacious in treating global symptoms of IBS.
The low-FODMAP diet is currently the most evidence-based diet intervention for IBS.
The low-FODMAP diet consists of the following three phases: 1) restriction (lasting no more than 4-6 weeks), 2) reintroduction of FODMAP foods and 3) personalization based on results from reintroduction.
Although observational studies found that most patients with IBS improve with a gluten-free diet, randomized controlled trials have yielded mixed results.
Read the full clinical guidance.