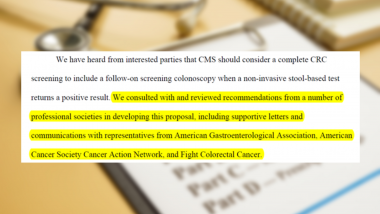
In a huge win for patients, Medicare will begin covering colonoscopies after a positive non-invasive stool test starting next year. Medicare was previously the only insurer who did not cover this critical prevention procedure.
This change comes after a year of advocacy led by AGA – including multiple meetings with senior officials at HHS and legislative pressure by members across the country.
Thank you to everyone in the GI community who advocated for this important change!
“Cost-sharing is a well-recognized barrier to screening and has resulted in disparities. Patients can now engage in CRC screening program and be confident that they will not face unexpected cost-sharing for colonoscopy after a positive non-invasive screening test,” says David Lieberman, MD, AGAF, who met with CMS officials multiple times to push this policy forward. “AGA knows that increased participation in screening will further reduce the burden of colorectal cancer.”
"This is a win for all patients and should elevate our nation’s screening rates while lowering the overall cancer burden, saving lives. Importantly, the CMS proposed rule changes will lessen colorectal cancer disparities eliminating a financial burden for many patients,” says AGA president John Carethers, MD, AGAF, who met with CMS earlier this month to advocate for this change.

“We would like to thank the American Cancer Society Cancer Action Network and Fight CRC, with whom AGA successfully partnered to eliminate out-of-pocket costs for all approved colorectal cancer screening strategies,” says John Inadomi, MD, AGAF, past president of AGA who spearheaded this initiative within AGA. “Previously for commercially insured patients, and now for patients covered by Medicare. The continuum is complete!”

Previous
Next