Gastroenterology Gastro Grand Rounds Case Study
A 68-year-old woman presented with abdominal pain, nausea and loss of appetite that progressively worsened over the month before presentation. She was in her usual state of health leading up to this presentation without any recent illnesses, travel, or new medications or supplements. Her past medical history was notable for a remote stroke, hypertension, migraine headaches, idiopathic urticaria, asthma, osteoarthritis, osteoporosis and recurrent urinary tract infections. Her surgical history included hysterectomy with bladder suspension 20 years ago. She had a known drug allergy to penicillin, causing hives. She was a nonsmoker and drank 1 alcoholic beverage 3–4 times a week. Her family history was notable for a brother who required surgery for liver cysts in adulthood and a younger brother with an enlarged liver. She had 3 healthy children. She did not take any herbal or dietary supplements. She has been on a stable medication regimen that included meloxicam for 1 year; clopidogrel, verapamil, and sumatriptan for 3 years; nitrofurantoin and alendronate for 4 years; and estrogen for 20 years.
On physical examination, she had a body mass index of 32 kg/m2, was afebrile and normotensive with a resting heart rate of 85 beats per minute and no respiratory distress. She was anicteric with an unremarkable head and neck examination, and no evidence of lymphadenopathy. Her cardiopulmonary examination was normal. Her abdomen was soft and nontender with no hepatosplenomegaly. She had no peripheral edema, no rash and no stigmata of chronic liver disease.
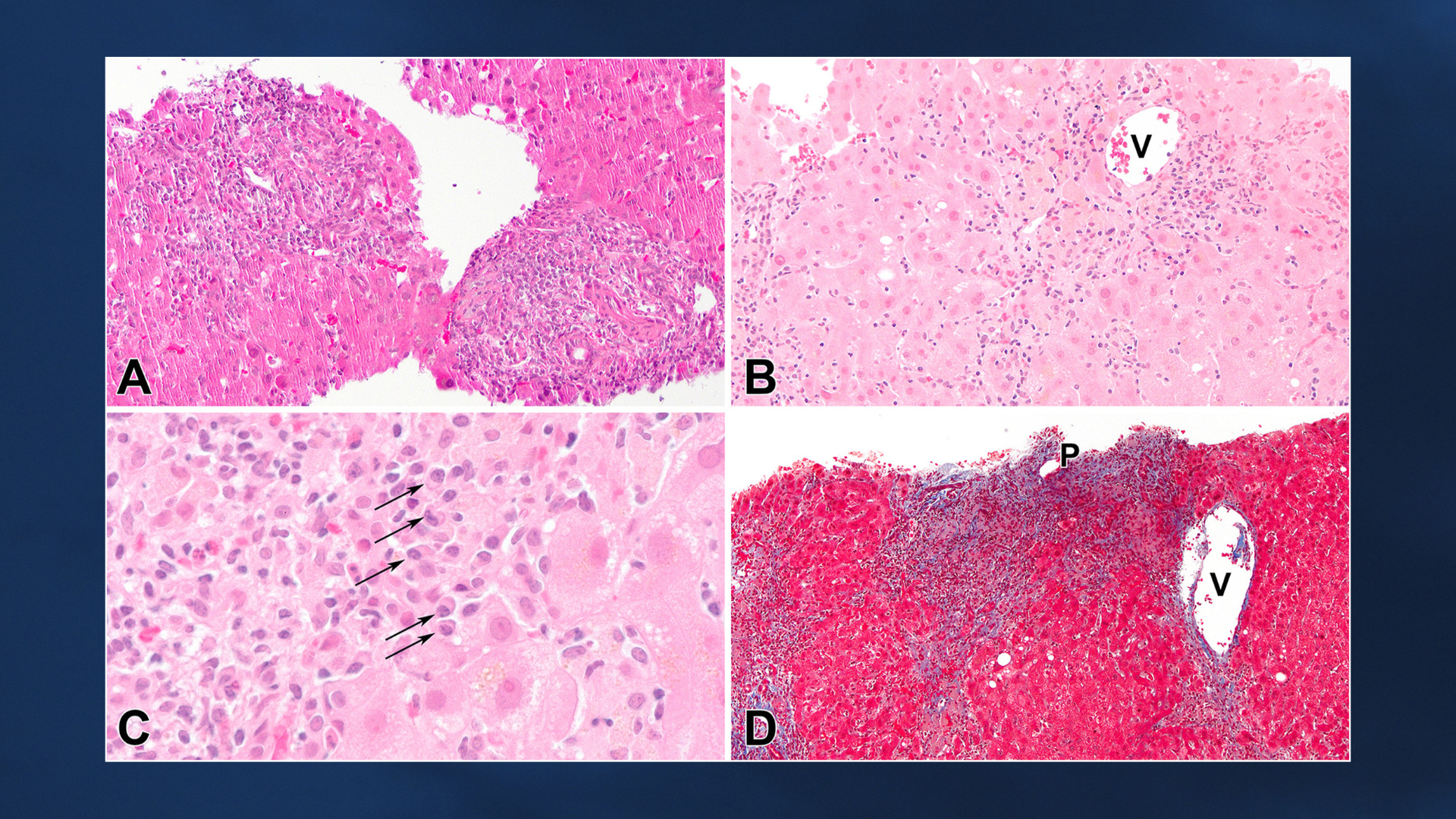
A liver biopsy was performed, which showed chronic hepatitis with severe interface hepatitis and portal to central bridging necrosis. The inflammation was predominantly lymphocytic with clusters of plasma cells at the interface and rare eosinophils. In addition to the bridging necrosis, there was perivenular inflammation and necrosis around many central veins. In areas of bridging necrosis there was early portal to central bridging fibrosis (Figure 1). Only minimal, macrovesicular steatosis was present without features of steatohepatitis. There was no bile duct injury or bile stasis.
Figure 1
What is the most likely etiology of the liver injury?
A. Idiopathic autoimmune hepatitis (AIH).
B. Drug-induced liver injury (DILI) from nitrofurantoin.
C. DILI from meloxicam.
D. DILI from alendronate