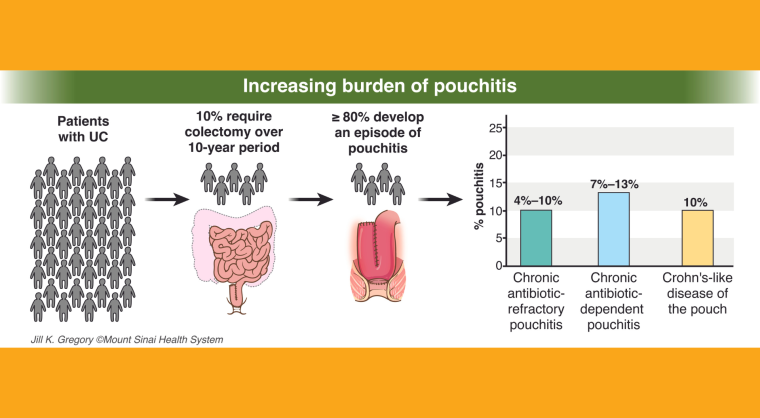
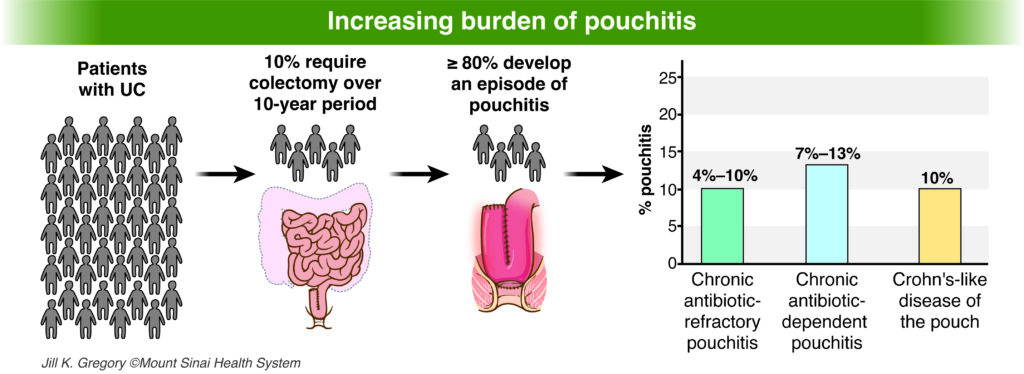
We have just released the first comprehensive evidence-based guideline on the management of pouchitis, the most common complication people with ulcerative colitis experience following surgery to remove their colon. The guideline was published today in Gastroenterology.
Treatment recommendations
- AGA suggests initial treatment of pouchitis with antibiotics.
- Treatment with multi-strain probiotics following an antibiotic course is suggested for preventing recurrent pouchitis.
- AGA suggests cyclical or near continuous antibiotic therapy to treat pouchitis that responds to antibiotics but recurs frequently and shortly after antibiotics are discontinued.
- In patients with recurrent pouchitis that doesn’t respond to antibiotics or Crohn’s-like disease of the pouch, AGA suggests advanced immunosuppressive medications (ie. Infliximab, vedolizumab, ustekinumab, upadacitinib, etc.)
Four types of inflammatory pouch disorders
This happens when a patient experiences infrequent episodes of pouchitis symptoms that get better with treatment.
This occurs when a patient’s pouchitis responds to antibiotics, but symptoms quickly return after antibiotics are stopped (typically within days to weeks).
This occurs when patients experience continuous symptoms of pouchitis that don’t get better with antibiotic therapy. Patients usually require more advanced treatment such as steroids or immunosuppressive medication.
Patients may have issues like fistulas (abnormal passages), strictures (narrowing) and inflammation in the small intestine above the pouch.