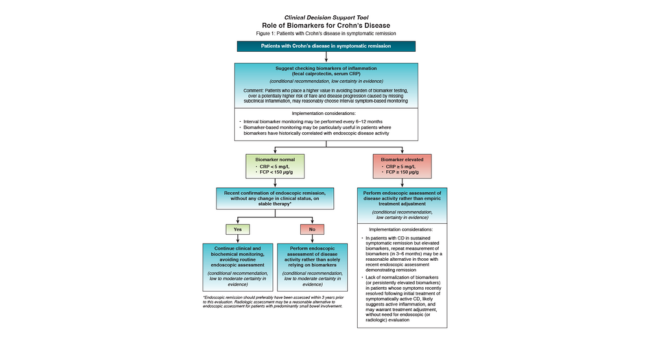
We just released a new evidence-based guideline recommending the use of blood and stool-based biomarkers to help manage Crohn’s disease. The guideline was published today in Gastroenterology.
Biomarkers are blood or stool tests that can give more information on an underlying disease process. In the context of IBD, biomarkers such as C-reactive protein (CRP) in blood and fecal calprotectin (FCP) in stool, can measure levels of inflammation. These levels can help you assess whether a patient’s Crohn’s disease is active or in remission.
AGA recommends the use of biomarkers in addition to colonoscopy and imaging studies.
"Patients’ symptoms do not always match endoscopic findings, so biomarkers are a useful tool to understand and monitor the status of inflammation and guide decision making in patients with Crohn's disease.”
For patients in remission:
- Check CRP and FCP every six to 12 months.
- These tests work best if CRP and FCP levels have previously matched with disease activity seen on endoscopic assessment.
For patients experiencing active symptoms:
- Check CRP and FCP every two to four months for patients experiencing an increase in symptoms (diarrhea and abdominal pain) to guide treatment adjustments.
- Before making any major treatment plan changes, consider repeating endoscopic or radiologic assessments.
For patients after surgery:
- FCP may be useful to monitor patients at low risk for disease recurrence.
- However, radiologic or endoscopic assessment should be performed when a post-operative recurrence is suspected rather than relying on biomarkers.
“Based on this guideline, biomarkers are no longer considered experimental and should be an integral part of IBD care. This is a win for Crohn’s disease patients. Biomarkers are usually easier to obtain, less invasive, more cost-effective than frequent colonoscopies and can be assessed more frequently for tighter disease control and better long-term outcomes in Crohn’s disease.”