AGA’s latest clinical practice update offers guidance on nonmalignant portal vein thrombosis (PVT) in patients with cirrhosis, including the role of direct oral anticoagulants and endovascular interventions. PVTs are common in patients with cirrhosis, affecting 11% over five years and are linked to advanced portal hypertension and mortality.
Watch as Drs. Jessica Davis and Fadi Francis discuss ways to manage PVT.
Best practice advice statements
- Asymptomatic patients with compensated cirrhosis do not require routine screening for PVT.
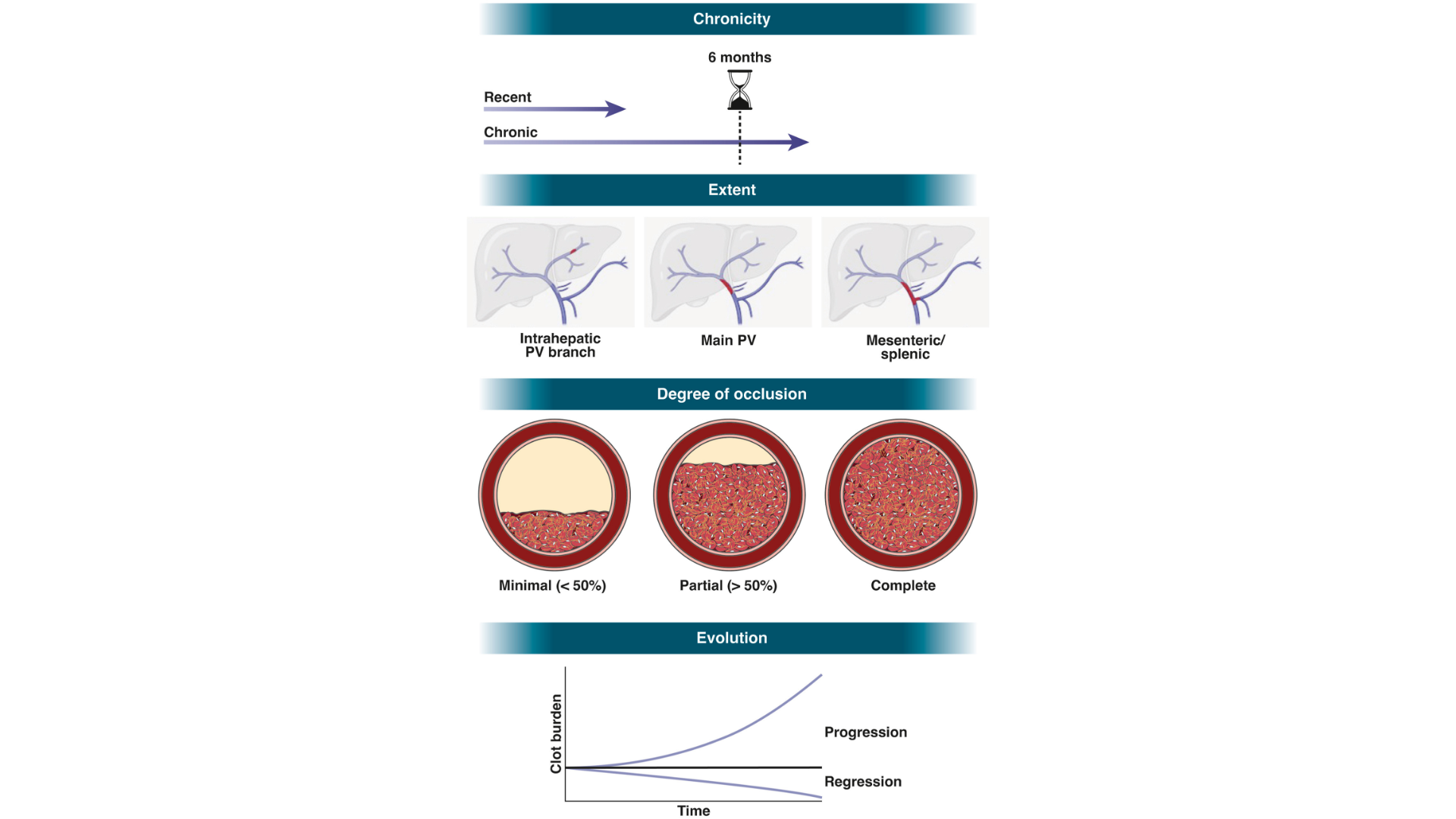
- Patients with cirrhosis with PVTs identified on Doppler ultrasound should undergo cross-sectional imaging with computed tomography or magnetic resonance imaging to confirm the diagnosis, evaluate for malignancy, and document the degree of lumen occlusion, clot extent, and chronicity.
- Patients with cirrhosis and PVT do not require a hypercoagulable workup in the absence of additional thromboemboli or, laboratory abnormalities, or family history suggestive of thrombophilia.
For all 11 best practice advice statements, read the full AGA Clinical Practice Update published in Gastroenterology.