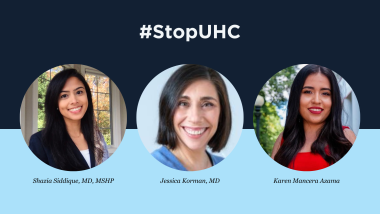
In a new editorial for The Well News, Dr. Shazia Siddique, chair-elect of the Government Affairs Committee, is raising concerns about barriers to care women face in the health care system.
Many women, Dr. Siddique notes, face an additional obstacle to care of having correctly prescribed treatments delayed or denied – the all-too-common insurance practice of prior authorization. Now, UnitedHealthcare’s (UHC) proposed “Gold Card” prior authorization program for 2024 poses to require insurance approval for nearly all endoscopies and colonoscopies, which would “be disastrous for patients.”


Dr. Jessica Korman, member of the Education and Training Committee, is also calling for insurers such as UHC to remove barriers to patient care in a new editorial for FierceHealthcare. She writes that UHC’s Advance Notification program is “merely a stepping-stone to the company’s future implementation of prior authorization” that is already an “administrative nightmare” and diverting time and resources from patient care.
Patient advocate Karen Mancera Azamar has experienced firsthand the detrimental effects from prior authorization. In a new editorial published by the Orlando Sentinel, Mancera shared how her insurance company refused to cover prescribed treatments for ulcerative colitis, and how the interruption in treatment led to severe symptoms and eventual hospitalization.
Patients should have timely access to GI care, but UHC’s current proposal sets up obstacles to second-guess doctors’ decisions and potentially lead to patients suffering, she writes. Unnecessary delays can lead to disease progression and a decreased quality of life – insurers cannot claim to prioritize patients’ well-being while making it harder to access needed care.