Clinical Gastroenterology and Hepatology image of the month:
While in the hospital for a severe coronavirus disease 2019 (COVID-19) infection, a 95-year-old woman developed hematemesis. She had been diagnosed 16 days prior and treated with remdesivir, dexamethasone and tocilizumab. Her comorbidities included chronic kidney disease stage 4, atrial fibrillation (not on anticoagulation), and chronic systolic heart failure. The patient was hypotensive (96/45 mmHg) and tachycardic (110 bpm). Laboratory studies demonstrated hemoglobin 8.5 g/dL (normal, 11.6–15.0 g/dL), compared with 11.2 g/dL 2 days prior.
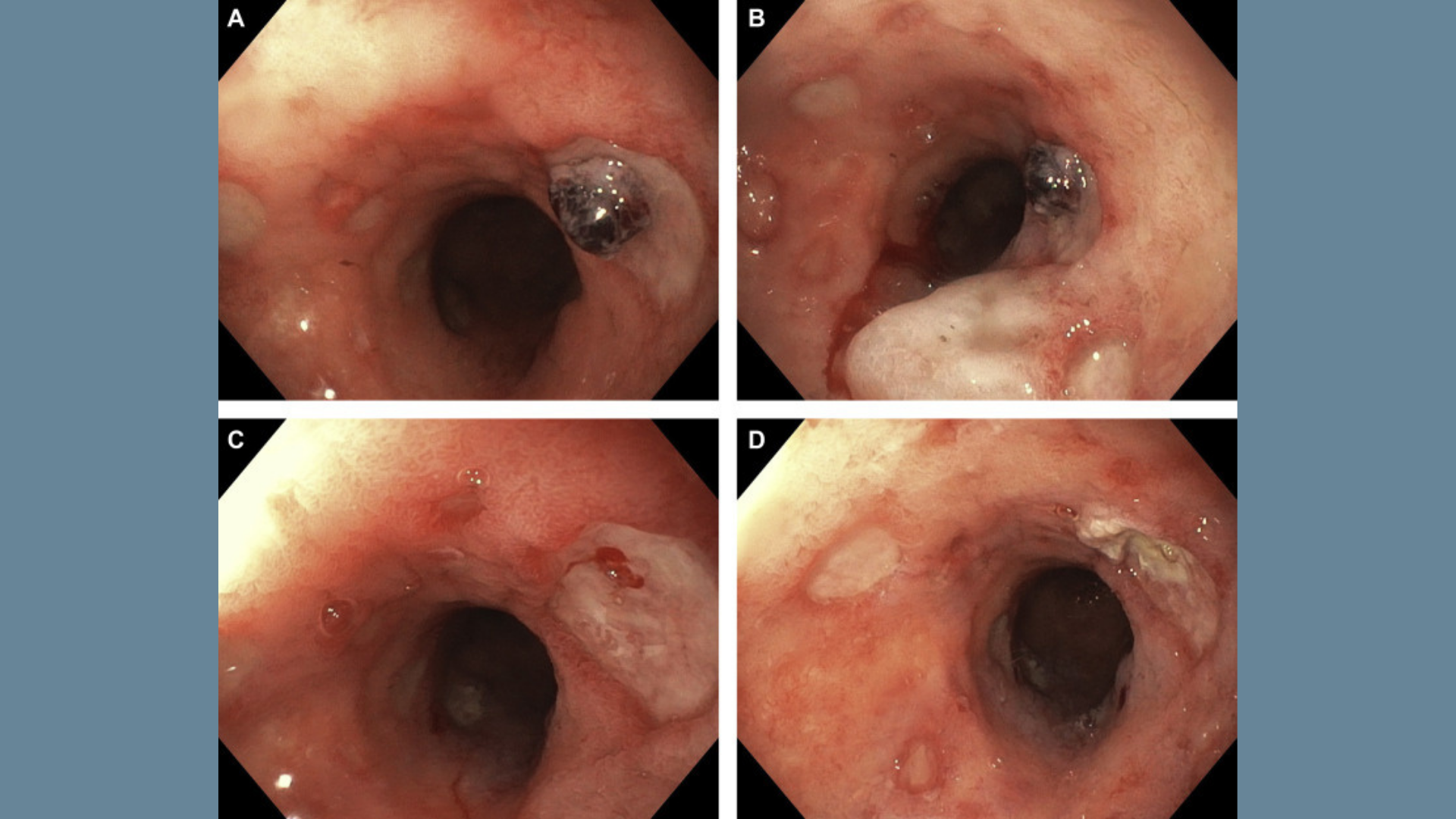
An esophagogastroduodenoscopy was performed and showed a 7-cm hiatal hernia and multiple cratered ulcers in the upper and middle esophagus, with the largest lesion measuring 15 mm. One of the ulcerations had an adherent clot (Figures A and B) with an underlying bleeding visible vessel (Figure C), which was treated with epinephrine injection and bipolar cauterization (Figure D). Biopsies taken from the center and periphery of esophageal ulcerations were negative for cytomegalovirus and herpes simplex virus but had detectable severe acute respiratory syndrome-associated coronavirus RNA. She had no recurrence of gastrointestinal bleeding.
This case highlights that esophageal ulcerations should be considered as a possible etiology of upper gastrointestinal bleeding in patients with COVID-19 infection.
View this case in the latest issue of Clinical Gastroenterology and Hepatology.