AGA’s new Clinical Practice Update provides seven best practice advice statements to guide your care of patients with early complications after bariatric/metabolic surgery.
They provide expert advice on flexible endoscopy as the principal method of treatment for patients within the 90-day overall complication period after undergoing surgery.
Read AGA Clinical Practice Update on Evaluation and Management of Early Complications After Bariatric/Metabolic Surgery: Expert Review, published in the August issue of Clinical Gastroenterology and Hepatology.
CLINICAL PRACTICE ADVICE
- Clinicians performing endoscopic approaches to treat early major postoperative complications should do so in a multidisciplinary manner with interventional radiology and bariatric/metabolic surgery co-managing the patient. Daily communication is advised.
- Clinicians should have a comprehensive knowledge of the indications, contraindications, risks, benefits and outcomes of each of the endoscopic treatment techniques. They should also have knowledge of the risks and benefits of alternative methods such as surgical and interventional radiological based approaches.
- Clinicians should have expertise in interventional endoscopy techniques, including but not limited to: using concomitant fluoroscopy, stent deployment and retrieval, managing stenosis, and managing percutaneous drains.
- Clinicians should screen all patients undergoing endoscopic management of bariatric/metabolic surgical complications and dietary intolerance for comorbid medical (nutrient deficiencies, infection, pulmonary embolism) and psychological (depression, anxiety) conditions.
- Endoscopic approaches to managing complications of bariatric/metabolic surgery may be considered for patients in the immediate, early and late postoperative periods depending on hemodynamic stability.
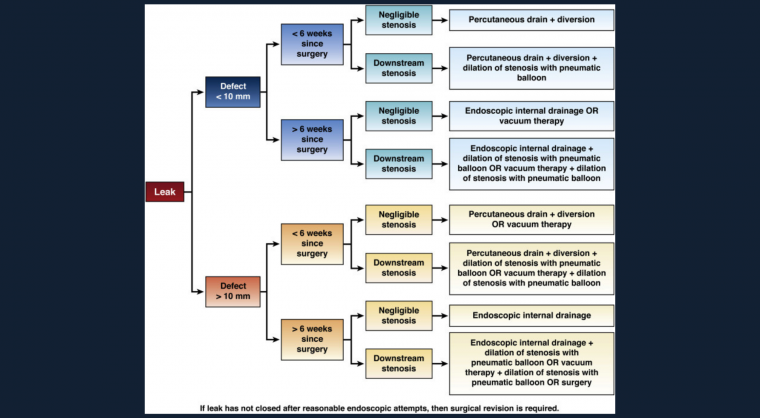
- Clinicians should have a detailed understanding of the pathophysiologic mechanisms initiating and perpetuating conditions such as staple-line leaks to allow for a prompt diagnosis and appropriate therapy to be targeted not only at the area of interest, but also any concomitant downstream stenosis.
- Endoscopic management of staple-line leaks are often not necessarily initial closure of the leak site, but rather techniques to promote drainage of material from the perigastric collection into the gastric lumen such that the leak site closes by secondary intention.