AGA’s new Clinical Practice Update provides 14 best practice advice statements for the prevention, detection and management of colorectal dysplasia in your patients with inflammatory bowel disease.
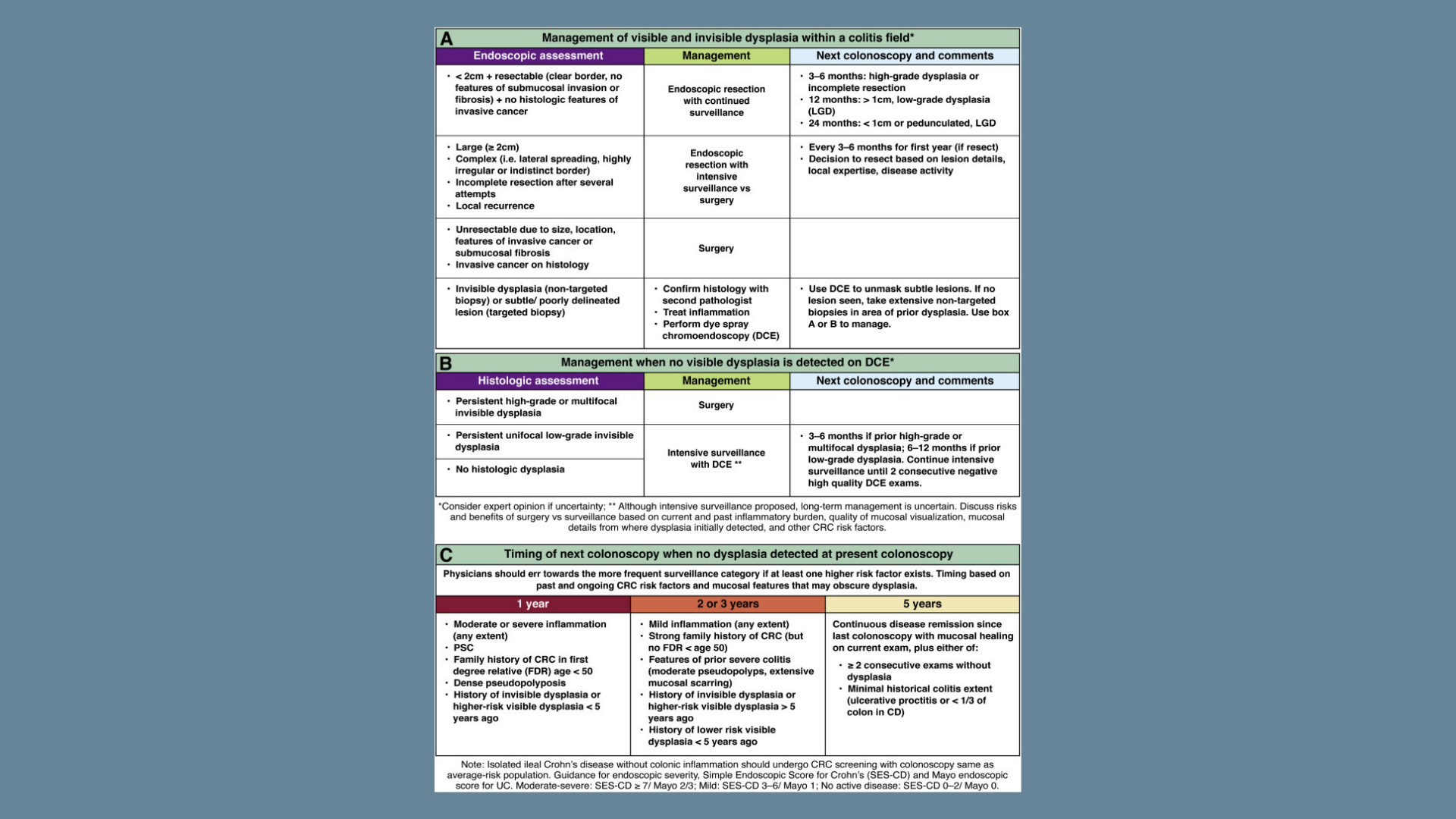
Over the years, IBD disease management and endoscopic technology has vividly shifted our mindset on how to treat IBD-related dysplasia. Nontargeted biopsy techniques and patient colectomy best practice advice in the setting of low-grade and/or invisible dysplasia are being increasingly challenged by technology-focused approaches that emphasize careful inspection and targeted sampling of visible and subtle lesions. AGA provides clear best practice statements on how to manage inflammatory bowel disease-related dysplasia using newer innovation techniques.
Best practice advice:
- Precancerous colorectal lesions in inflammatory bowel disease should be described as either polypoid, nonpolypoid, or invisible using a modified Paris Classification.
- Screening should begin 8-10 years after the initial diagnosis unless there are underlying primary sclerosing cholangitis in which case screening should start immediately.
- Chromoendoscopy should be considered in all IBD patients with virtual chromoendoscopies being a suitable alternative when using HD colonoscopy
- Nontargeted biopsies should be considered if chromoendoscopy is not utilized, but you may consider doing both chromoendoscopy and non-targeted biopsies in high risk cases like primary sclerosing cholangitis
- Following a negative screening, colonoscopy surveillance should be performed every 1-5 years depending on individual patient’s risk factors
To view the entire list of best practice statements, read AGA Clinical Practice Update on Endoscopic Surveillance and Management of Colorectal Dysplasia in Inflammatory Bowel Diseases: Expert Review, published in the September issue of Gastroenterology.