AGA has published a new clinical practice update on the use of endoscopic scoring systems for assessing mucosal healing in patients with inflammatory bowel disease (IBD), including ulcerative colitis and Crohn’s disease.
The big takeaway
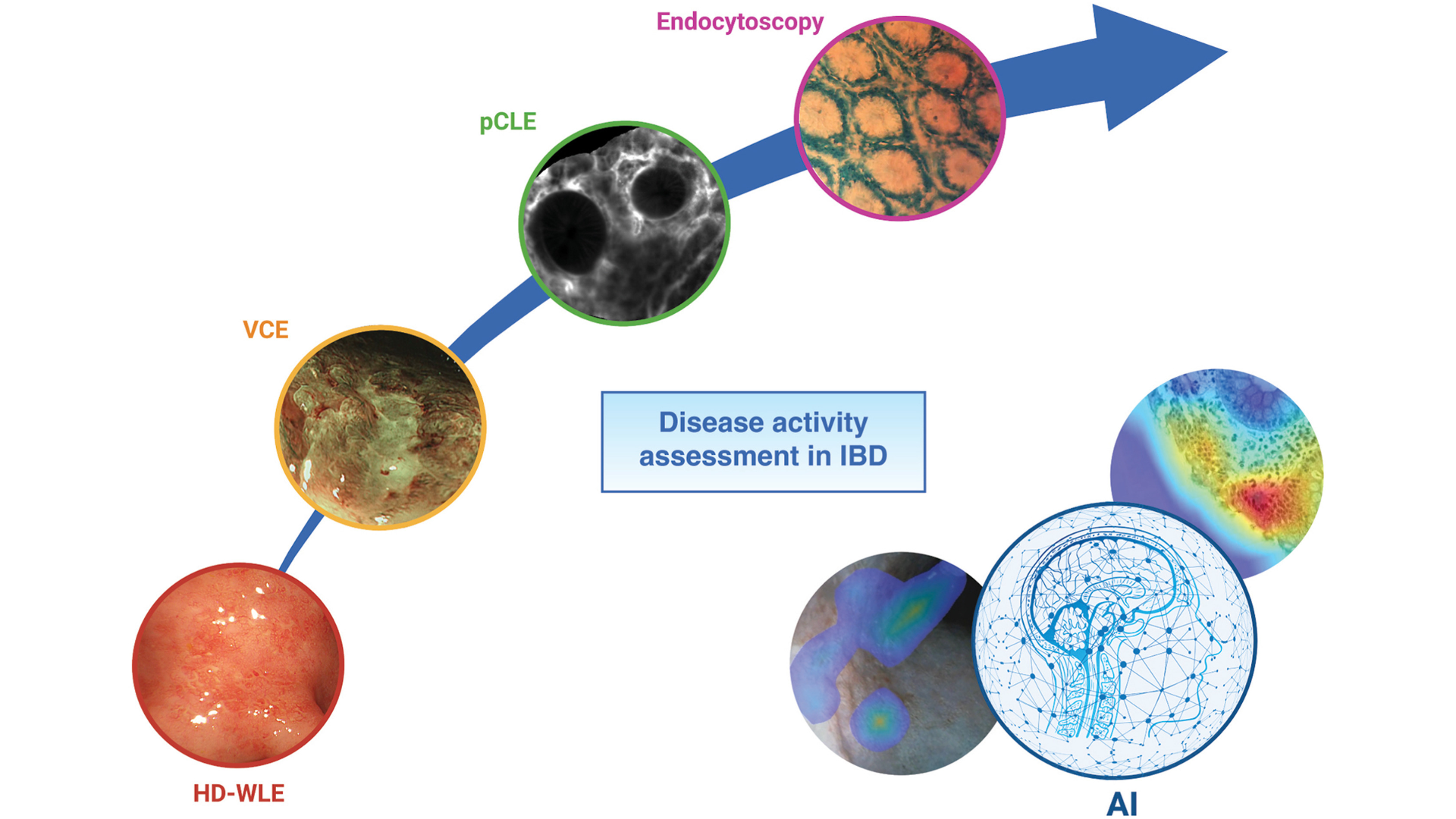
Endoscopic scoring systems provide objectivity, uniformity, and standardization in reporting mucosal appearance, enhancing clinical decision-making for treatment strategies and improving patient outcomes. Despite some limitations — such as complexity, subjectivity, and limited validation — these scoring systems remain integral to clinical practice. Training and online resources can support more widespread use by gastroenterologists, while AI systems may further refine scoring accuracy and standardization.
Current scoring systems include:
- Mayo Endoscopic Score (MES)
- Ulcerative Colitis Endoscopic Index of Severity (UCEIS)
- Crohn’s Disease Endoscopic Index of Severity (CDEIS)
- Simple Endoscopic Score for CD (SES-CD)
- Rutgeert’s score is used to assess inflammation recurrence post-surgery.
- Endoscopy is essential for evaluating disease activity, treatment response, and predicting outcomes in IBD. Mucosal healing is now a critical treatment goal.
- Standardizing scoring systems and increasing GI training remain key challenges.
- Virtual chromoendoscopy (VCE): Provides enhanced visualization, which may improve differentiation between remission and mild disease (e.g., PICaSSO score).
- Artificial intelligence: Holds promise for improved accuracy and consistency in endoscopic scoring.
Hear from the experts
Drs. Anna M. Buchner and Marietta Iacucci discuss the importance of endoscopic scoring systems.
Read the full AGA clinical practice update on endoscopic scoring systems for assessing mucosal healing in patients with IBD in the November issue of Clinical Gastroenterology and Hepatology.
Do you value this clinical information?
Ensure you keep receiving it by renewing your AGA membership or becoming a member.