Gastric cancer is a leading cause of preventable cancer-related deaths in certain U.S. populations. AGA’s new clinical practice update guides primary prevention strategies, including H. pylori eradication and secondary prevention through endoscopic screening and surveillance of precancerous conditions such as gastric intestinal metaplasia (GIM).
Watch as Drs. Andrew Yang and Shailja Shah discuss the latest best practices for managing patients at high risk for gastric cancer.
Best practice advice statements
- There are identifiable high-risk groups in the U.S. who should be considered for gastric cancer screening. These include first-generation immigrants from high-incidence regions and possibly other non-White racial and ethnic groups, those with a family history of gastric cancer in a first-degree relative, and individuals with certain hereditary gastrointestinal polyposis or hereditary cancer syndromes.
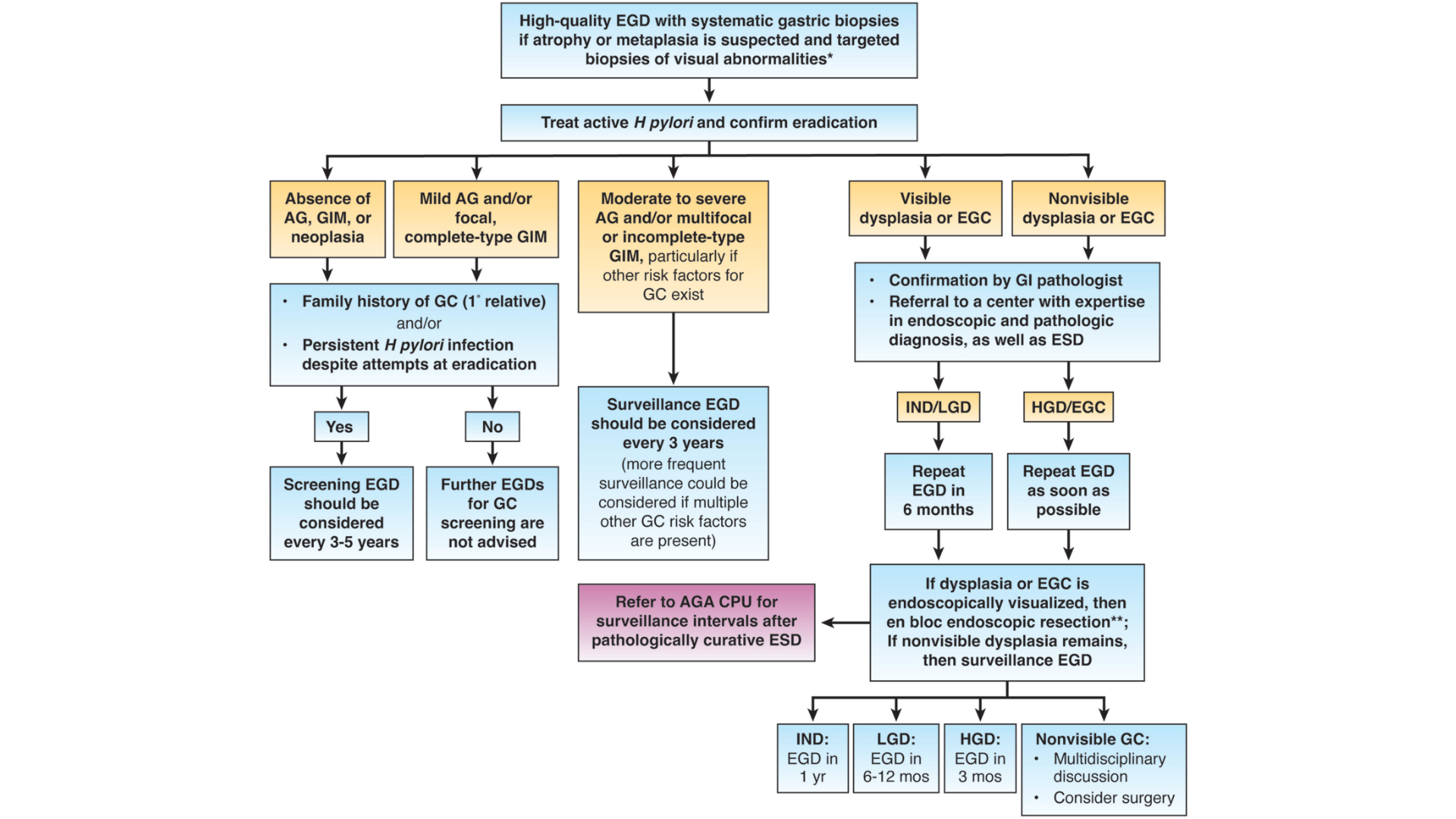
- Endoscopy is the best test for screening or surveillance in individuals at increased risk for gastric cancer. Endoscopy enables direct visualization to endoscopically stage the mucosa and identify areas concerning for neoplasia, as well as enables biopsies for further histologic examination and mucosal staging. Both endoscopic and histologic staging are key for risk stratification and determining whether ongoing surveillance is indicated and at what interval.
- High-quality upper endoscopy for the detection of premalignant and malignant gastric lesions should include the use of a high-definition white-light endoscopy system with image enhancement, gastric mucosal cleansing, and insufflation to achieve optimal mucosal visualization, in addition to adequate visual inspection time, photodocumentation, and use of a systematic biopsy protocol for mucosal staging when appropriate.
For all 15 best practice advice statements, read the full AGA Clinical Practice Update published in Gastroenterology.