Exocrine pancreatic insufficiency (EPI) is caused by a failure of the pancreas to deliver the necessary level of specific pancreatic digestive enzymes to the intestine, leading to the maldigestion of nutrients and macronutrients resulting in subsequent deficiencies.
EPI is frequently underdiagnosed, leading patients to be undertreated.
Author Anna Buchner, MD, PhD, provides an overview of this new clinical guidance, and the best practice advice statements clinicians should be taking into their practice.
Key takeaways
-
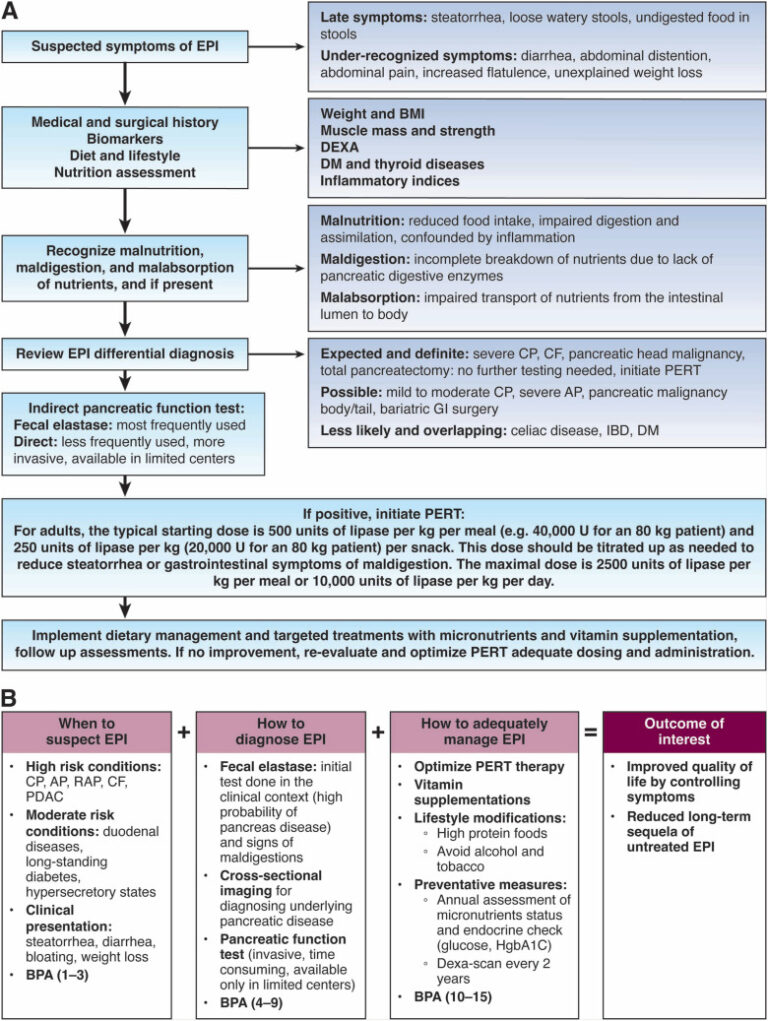
EPI should be suspected in patients with high-risk clinical conditions (i.e. chronic pancreatitis, relapsing acute pancreatitis, pancreatic ductal adenocarcinoma, cystic fibrosis and previous pancreatic surgery) and considered in patients with moderate-risk clinical conditions (i.e. celiac disease, duodenal Crohn’s disease, previous intestinal surgery, diabetes mellitus and Zollinger-Ellison syndrome).
-
Patients with EPI can present with symptoms such as: steatorrhea with or without diarrhea, weight loss, bloating, excessive flatulence, fat-soluble vitamin deficiencies and protein-calorie malnutrition.
-
To diagnose EPI, fecal elastase test performed on either a semi-solid or solid stool specimen is the most appropriate initial test. A fecal elastase level <100 μg/g provides good evidence of EPI. Levels of 100–200 μg/g are indeterminate for EPI and warrant a further workup.
-
Treatment with pancreatic enzyme replacement therapy (PERT) is required in patients diagnosed with EPI. PERT should be taken during every meal (including snacks) at a dose of at least 40,000 USP units of lipase per meal and 20,000 units per snack to start. If EPI is left untreated, it will result in complications related to fat malabsorption and malnutrition, having a negative impact on quality of life.
Read the full AGA Clinical Practice Update on the Epidemiology, Evaluation, and Management of Exocrine Pancreatic Insufficiency: Expert Review, published in the November issue of Gastroenterology.
See the full 15 best practice advice statements on our clinical guidance page.