1. Diet advice is ideally prescribed to patients with irritable bowel syndrome (IBS) who have insight into their meal-related gastrointestinal symptoms and are motivated to make the necessary changes. To optimize the quality of teaching and clinical response, referral to a registered dietitian nutritionist (RDN) should be made to patients who are willing to collaborate with an RDN and patients who are not able to implement beneficial dietary changes on their own. If a gastrointestinal RDN is not available, other resources can assist with implementation of diet interventions.
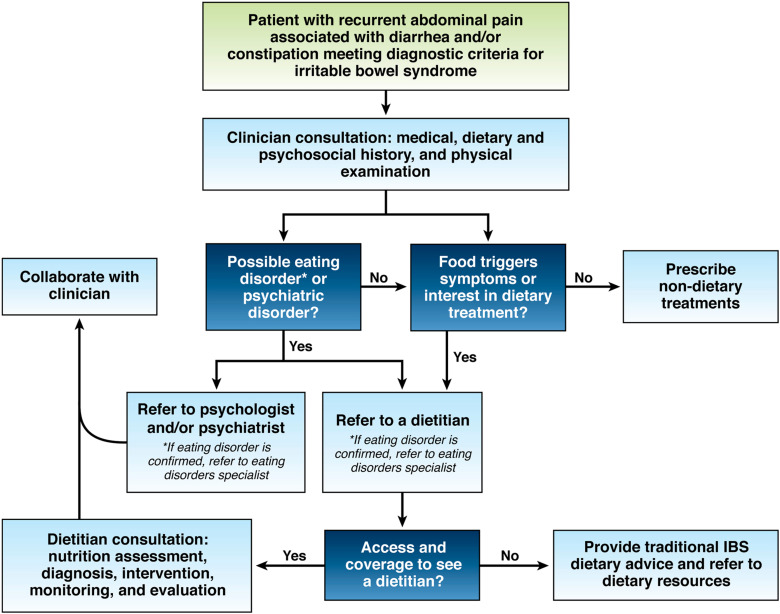
2. Patients with IBS who are poor candidates for restrictive diet interventions include those consuming few culprit foods, those at risk for malnutrition, those who are food insecure and those with an eating disorder or uncontrolled psychiatric disorder. Routine screening for disordered eating or eating disorders by careful dietary history is critical because they are common and often overlooked in gastrointestinal conditions.
3. Patients should attempt specific IBS diet interventions for a predetermined length of time. If the patient has no clinical response, the diet intervention should be abandoned for another treatment alternative, for example, a different diet, medication or other form of therapy.
4. In preparation for a visit with an RDN, patients should provide dietary information that will assist in developing an individualized nutrition care plan.
5. Soluble fiber is efficacious in treating global symptoms of IBS.
6. The low-FODMAP diet is currently the most evidence-based diet intervention for IBS. Healthy eating advice as described by the National Institute of Health and Care Excellence Guidelines, among others, also offers benefit to a subset of patients with IBS.
7. The low-FODMAP diet consists of the following 3 phases: 1) restriction (lasting no more than 4-6 weeks), 2) reintroduction of FODMAP foods and 3) personalization based on results from reintroduction.
8. Although observational studies found that most patients with IBS improve with a gluten-free diet, randomized controlled trials have yielded mixed results.
9. There are limited data showing that selected biomarkers can predict response to diet interventions in patients with IBS, but there is insufficient evidence to support their routine use in clinical practice.