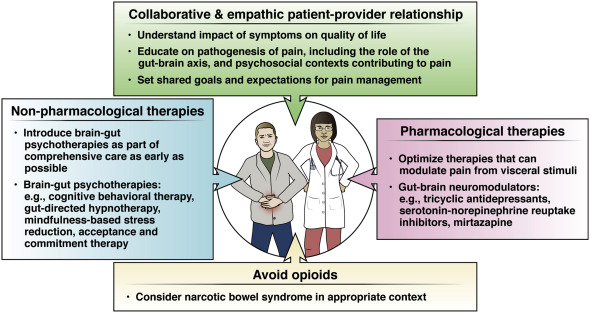
1. Effective management of persistent pain in disorders of gut-brain interaction requires a collaborative, empathic, culturally sensitive patient-provider relationship.
2. Providers should master patient-friendly language about the pathogenesis of pain, leveraging advances in neuroscience and behavioral science. Providers must also understand the psychological contexts in which pain is perpetuated.
3. Opioids should not be prescribed for chronic GI pain due to a disorder of gut-brain interaction. If patients are referred on opioids, these medications should be prescribed responsibly, via multidisciplinary collaboration, until they can be discontinued.
4. Non-pharmacological therapies should be considered routinely as part of comprehensive pain management, and ideally brought up early on in care.
5. Providers should optimize medical therapies that are known to modulate pain and be able to differentiate when GI pain is triggered by visceral factors vs. centrally mediated factors.
6. Providers should familiarize themselves with a few effective neuromodulators, knowing the dosing, side effects and targets of each and be able to explain to the patient why these drugs are used for the management of persistent pain.