1. The role of a gastroenterologist in patients referred for evaluation of suspected extra esophageal symptom is to assess for gastroesophageal etiologies that could contribute to the presenting symptoms.
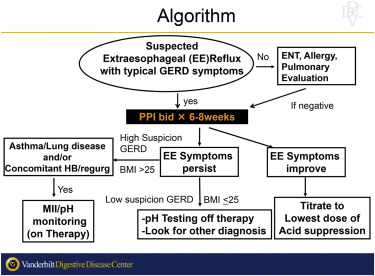
2. Non-GI evaluations by ear, nose and throat (ENT), pulmonary and/or allergy are essential and often should be performed initially in most patients as the cause of the extraesophageal symptom is commonly multifactorial or not esophageal in origin.
3. Empiric therapy with aggressive acid suppression for 6-8 weeks with special focus on response of the extraesophageal symptoms can help in assessing association between reflux and extraesophageal symptoms.
4. No single testing methodology exists to definitively identify reflux as the etiology for the suspected extra esophageal symptoms.
5. Constellation of patient presentation, diagnostic test results and response to therapy should be employed in the determination of reflux as a possible etiology in extra esophageal symptoms.
6. Testing may need to be off or on proton pump inhibitor (PPI) therapy depending on patients’ presenting demographics and symptoms in assessing the likelihood of abnormal gastroesophageal reflux.
A. On therapy testing may be considered in those with high probability of baseline reflux (those with previous esophagitis, Barrett’s esophagus or abnormal pH).
B. Off therapy testing may be considered in those with low probability of baseline reflux with the goal of identifying moderate to severe reflux at baseline.
7. Lack of response to aggressive acid suppressive therapy combined with normal pH testing off therapy or impedance-pH testing on therapy significantly reduces the likelihood that reflux is a contributing etiology in presenting extraesophageal symptoms.
8. Surgical fundoplication is discouraged in those with extra esophageal reflux symptoms unresponsive to aggressive PPI therapy.
9. Fundoplication should only be considered in those with a mechanical defect (e.g., hiatal hernia), moderate to severe reflux at baseline off PPI therapy who have continued reflux despite PPI therapy and have failed more conservative non-GI treatments.