1. Review histologic findings with experienced pathologists who specialize in gastroenterology.
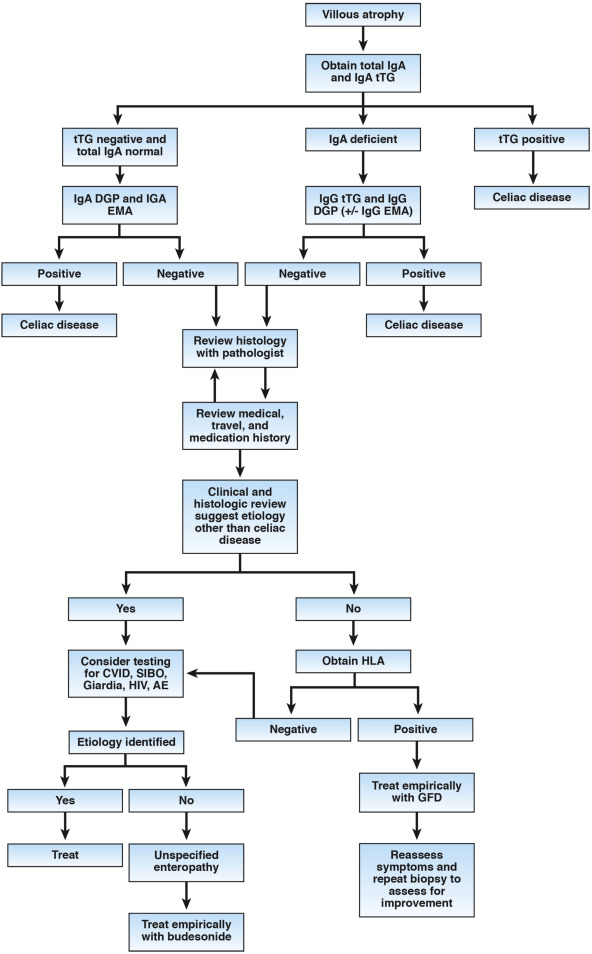
2. Serologic tests are essential for an accurate diagnosis of celiac disease. For patients with suspected celiac disease but negative results from serologic tests, total IgA level should be measured; patients should also be tested for anti-tissue transglutaminase, IgA against deamidated gliadin peptide, and endomysial antibody (IgA). Patients with total IgA levels below the lower limit of detection and IgG against tissue transglutaminase or deamidated gliadin peptide, or endomysial antibody, should be considered to have celiac disease with selective IgA deficiency rather than seronegative celiac disease.
3. Patients’ diets should be carefully reviewed and duodenal biopsies should be collected and analyzed at the time of serologic testing to determine exposure to gluten and accuracy of test results.
4. Thorough medication histories should be collected from patients, with attention to angiotensin II receptor blockers, such as olmesartan, along with travel histories to identify potential etiologies of villous atrophy. This will guide additional testing.
5. Patients should be analyzed for disease-associated variants in human leukocyte antigen genes; results must be carefully interpreted. Negative results can be used to rule out celiac disease in seronegative patients.
6. Patients with suspected celiac disease who are seronegative but have villous atrophy and genetic risk factors for celiac disease must undergo endoscopic evaluation after 1-3 years on a gluten-free diet to evaluate improvements in villous atrophy. A diagnosis of seronegative celiac disease can then be confirmed based on clinical and histologic markers of improvement on the gluten-free diet.
7. Seronegative patients with an identified cause for enteropathy should be treated accordingly; a follow-up biopsy might or might not be necessary.
8. Patients with persistent signs and symptoms who do not respond to a gluten-free diet, and for whom no etiology of enteropathy is ultimately identified, should be treated with budesonide.