Lesion assessment
1. Recommend the documentation of endoscopic descriptors of the lesion, including location, size in millimeters, and morphology in the colonoscopy procedure report.
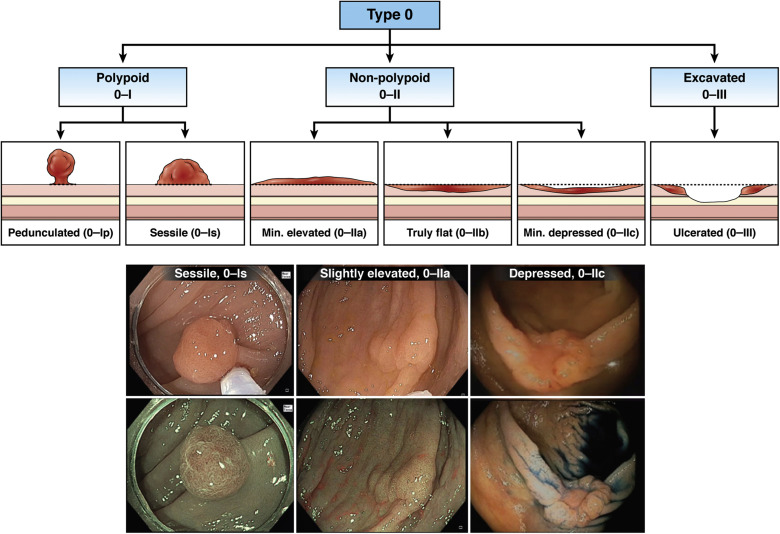
2. Suggest the use of the Paris classification to describe the surface morphology in order to provide a common nomenclature.
3. Suggest that for non-pedunculated adenomatous (Paris 0-II and 0-Is) lesions ≥10 mm, surface morphology should be also described as granular or non-granular lateral spreading lesions.
4. Recommend photo documentation of all lesions ≥10 mm in size before removal, and suggest photo documentation of the post-resection defect.
5. Suggest proficiency in the use of electronic- (eg, narrow-band imaging [NBI], i-scan, Fuji Intelligent Chromo Endoscopy or blue light imaging) or dye (chromoendoscopy)-based image enhanced endoscopy techniques to apply optical diagnosis classifications for colorectal lesion histology.
6. Recommend proficiency in the endoscopic recognition of deep submucosal invasion.
Removal techniques
1. Recommend cold snare polypectomy to remove diminutive (≤5 mm) and small (6–9 mm) lesions due to high complete resection rates and safety profile.
2. Recommend against the use of cold forceps polypectomy to remove diminutive (≤5 mm) lesions due to high rates of incomplete resection. For diminutive lesions ≤2 mm, if cold snare polypectomy is technically difficult, jumbo or large-capacity forceps polypectomy may be considered.
3. Recommend against the use of hot biopsy forceps for polypectomy of diminutive (≤5 mm) and small (6-9 mm) lesions due to high incomplete resection rates, inadequate histopathologic specimens, and complication rates.
4. Suggest cold or hot snare polypectomy (with or without submucosal injection) to remove 10–19 mm non-pedunculated lesions.
5. Recommend EMR as the preferred treatment method of large (≥20 mm) non-pedunculated colorectal lesions. Endoscopic resection can provide complete resection and obviate the higher morbidity, mortality and cost associated with alternative surgical treatment.
6. Recommend an endoscopist experienced in advanced polypectomy to manage large (≥20 mm) non-pedunculated colorectal lesions.
7. Recommend snare resection of all grossly visible tissue of a lesion in a single colonoscopy session and in the safest minimum number of pieces, as prior failed attempts at resection are associated with higher risk for incomplete resection or recurrence.
8. Suggest the use of a contrast agent, such as indigo carmine or methylene blue, in the submucosal injection solution to facilitate recognition of the submucosa from the mucosa and muscularis propria layers.
9. Recommend against the use of tattoo, using sterile carbon particle suspension, as the submucosal injection solution. The carbon particle suspension may result in submucosal fibrosis, and can thus reduce the technical success of future endoscopic resection of residual or recurrent lesion.
10. Suggest the use of a viscous injection solution (eg, hydroxyethyl starch, Eleview, ORISE Gel) for lesions ≥20 mm to removal the lesion in fewer pieces and less procedure time compared to normal saline.
11. Recommend against the use of ablative techniques (eg, argon plasma coagulation [APC], snare tip soft coagulation) on endoscopically visible residual tissue of a lesion, as they have been associated with an increased risk of recurrence.
12. Suggest the use of adjuvant thermal ablation of the post-EMR margin, where no endoscopically visible adenoma remains despite meticulous inspection. There is insufficient evidence to recommend a specific modality (ie, APC, snare tip soft coagulation) at this time.
13. Recommend detailed inspection of the post-resection mucosal defect to identify features for immediate or delayed perforation risk, and perform endoscopic clip closure, accordingly.
14. Suggest prophylactic closure of resection defects ≥20 mm in size in the right colon, when closure is feasible.
15. Suggest treatment of intraprocedure bleeding using endoscopic coagulation (eg, coagulation forceps or snare-tip soft coagulation) or mechanical therapy (eg, clip), with or without the combined use of dilute epinephrine injection.
16. Suggest that patients on anti-thrombotics who are candidates for endoscopic removal of a colorectal lesion ≥20 mm receive individualized assessment, balancing the risks of interrupting anticoagulation for colonoscopic polypectomy or mucosal resection against the risks of significant bleeding during and after the procedure.
17. Recommend hot snare polypectomy to remove pedunculated lesions ≥10 mm.
18. Recommend prophylactic mechanical ligation of the stalk with a detachable loop or clips on pedunculated lesions with head ≥20 mm or with stalk thickness ≥5 mm to reduce immediate and delayed post-polypectomy bleeding.
19. Suggest retrieval of large pedunculated polyp specimens en bloc to ensure ability to assess resection margins, rather than dividing polyp heads to facilitate through the scope specimen retrieval.
Lesion marking
1. Recommend the use of tattoo, using sterile carbon particle suspension, to demarcate any lesion that may require localization at future endoscopic or surgical procedures.
2. Suggest placing the tattoo at 2-3 separate sites located 3-5 cm anatomically distal to the lesion (anal side), particularly when the purpose is to mark the lesion for later endoscopic resection. The carbon particle suspension if injected at or in close approximation to the lesion, may result in submucosal fibrosis, and can thus reduce the technical success and increase the risk of future endoscopic resection.
3. Suggest endoscopists and surgeons establish a standard location of tattoo injection relative to the colorectal lesion of interest at their institution.
4. Recommend documentation of the details of the tattoo injection (ie, material, volume, position relative to the lesions) in the colonoscopy report, as well as photo documentation of the tattoo in relation to the colorectal lesion.
Surveillance
1. Recommend intensive follow-up schedule in patients after piecemeal EMR (lesions ≥20 mm) with the first surveillance colonoscopy at 6 months, and the intervals to the next colonoscopy at 1 year and then 3 years.
2. To assess for local recurrence, we suggest careful examination of the post-mucosectomy scar site using enhanced imaging, such as dye-based (chromoendoscopy) or electronic-based methods, as well as obtaining targeted biopsies of the site. Post-resection scar sites that show both normal macroscopic and microscopic (biopsy) findings have the highest predictive value for long-term eradication.
3. In surveillance cases with suspected local recurrence, we suggest endoscopic resection therapy with repeat EMR, snare or avulsion method, and consider ablation of the perimeter of the post-treatment site. In such cases, subsequent examinations should be performed at 6-12 months until there is no local recurrence. Once a clear resection site is documented by endoscopic assessment and histology, the next follow-ups are performed at 1-year and then 3-year intervals.
4. In addition to detailed inspection of the post-mucosectomy scar site, recommend detailed examination of the entire colon at the surveillance colonoscopy to assess for synchronous colorectal lesions.
Equipment
1. Recommend the use of carbon dioxide insufflation instead of air during colonoscopy and EMR.
2. Suggest the use of microprocessor-controlled electrosurgical units.
Quality of Polypectomy
1. When an endoscopist encounters a suspected benign colorectal lesion that he or she is not confident to remove completely, recommend referral to an endoscopist experienced in advanced polypectomy for subsequent evaluation and management, in lieu of referral for surgery.
2. Suggest the documentation of the type of resection method (eg, cold snare, hot snare, EMR) used for the colorectal lesion removal in the procedure report.
3. Recommend that non-pedunculated lesions with endoscopic features suggestive of submucosal invasive cancer and that are resected en bloc be retrieved and pinned to a flat surface before submitting the specimen to the pathology laboratory to facilitate pathologic sectioning that is perpendicular to the resection plane.
4. For non-pedunculated colorectal lesions resected en bloc with submucosal invasion, recommend that pathologists measure and report the depth of invasion, distance of the cancer from the vertical and lateral resection margin, in addition to prognostic histologic features, such as degree of differentiation, presence or absence of lymphovascular invasion, and tumor budding.
5. Recommend that endoscopists resect pedunculated lesions en bloc, and that when submucosal invasion is present, pathologists report the distance of cancer from the cautery line, the degree of tumor differentiation, and presence or absence of lymphovascular invasion.
6. Recommend endoscopists engage in a local (institution-, hospital- or practice-based) quality-assurance program, including measuring and reporting of post-polypectomy adverse events.
7. Suggest measuring and reporting the proportion of patients undergoing colonoscopy who are referred to surgery for benign colorectal lesion management.
8. Suggest the use of polypectomy competency assessment tools, such as Direct Observation of Polypectomy Skills and/or the Cold Snare Polypectomy Competency Assessment Tool in endoscopic training programs, and in practice improvement programs.