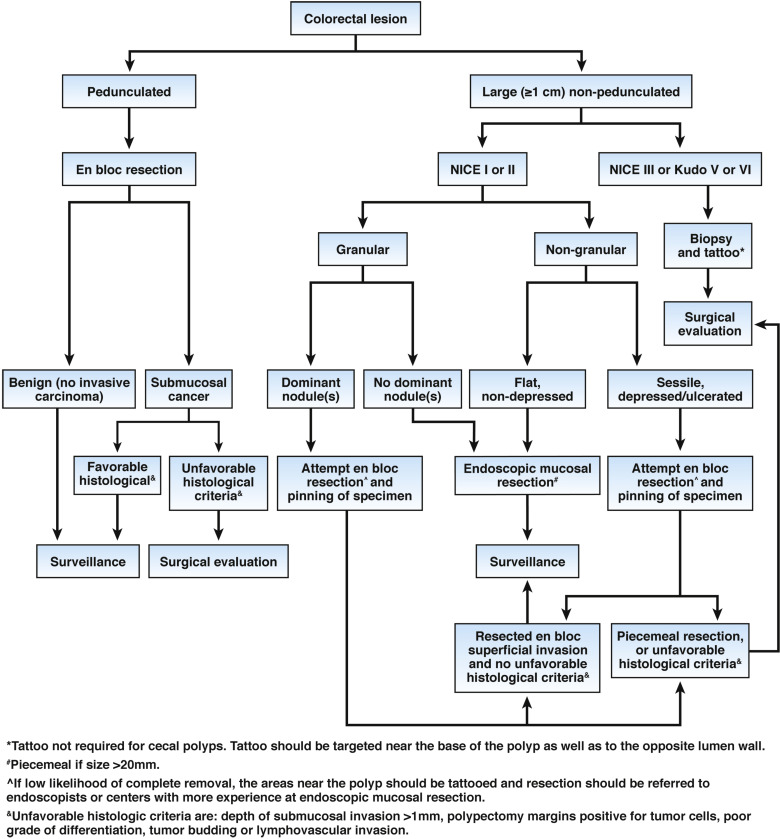
1a. The task force recommends that both pedunculated and nonpedunculated polyps with the following features be considered to have deep submucosal invasion: NICE classification type 3 or Kudo classification of type V (VN and VI).
1b. Nonpedunculated lesions with these features should be biopsied (in the area of surface feature disruption), tattooed (unless in or near the cecum), and referred to surgery. Pedunculated polyps with features of deep submucosal invasion should undergo endoscopic polypectomy.
2a. LST-NG morphology with sessile shape or depression, and LST-G with a dominant nodule predict a higher risk of submucosally invasive cancer.
2b. The task force recommends that such lesions be considered for en bloc endoscopic resection, instead of piecemeal resection, when feasible and based on local expertise. In the case of LST-G with a dominant nodule, at least the nodular area should be considered for en bloc resection. All pedunculated polyps, even if large, should be resected en bloc.
3. The task force recommends that specimens with features associated with submucosally invasive cancer that are removed en bloc be handled in ways to optimize specimen orientation and pathologic assessment.
4a. The task force recommends that nonpedunculated malignant polyps be considered high risk for residual or recurrent cancer if they have any of the following features: poor tumor differentiation, lymphovascular invasion, submucosal invasion depth >1 mm, tumor involvement of the cautery margin, or tumor budding.
4b. The task force recommends that pedunculated malignant polyps be considered at high risk of residual or recurrent cancer if they have any of the following features: poor tumor differentiation, lymphovascular invasion, tumor within 1 mm of the resection margin.
5. The task force recommends that the pathology report adhere to the recommendation of the College of American Pathologists structured template and that the report contain the histologic type, grade of differentiation, tumor extension/invasion, stalk and mucosal margin status, as well as the presence or absence of lymphovascular invasion. We suggest other aspects, such as specimen integrity, polyp size, polyp morphology and tumor budding be included.
6. The task force suggests establishing methods of communication among the gastroenterologist, pathologist, oncologist, surgeon and the patient for the management of patients with malignant polyps.