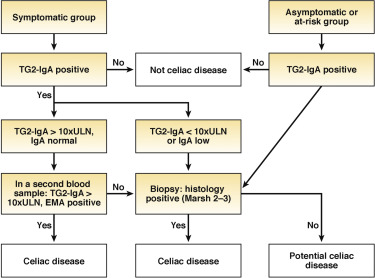
1. Serology is a crucial component of the detection and diagnosis of celiac disease, particularly tissue transglutaminase-immunoglobulin A (TG2-IgA), IgA testing, and less frequently, endomysial IgA testing.
2. Thorough histological analysis of duodenal biopsies with Marsh classification, counting of lymphocytes per high-power field, and morphometry is important for diagnosis as well as for differential diagnosis.
2a. TG2-IgA, at high levels (> ×10 upper normal limit) is a reliable and accurate test for diagnosing active celiac disease. When such a strongly positive TG2-IgA is combined with a positive endomysial antibody in a second blood sample, the positive predictive value for celiac disease is virtually 100%. In adults, esophagogastroduodenoscopy (EGD) and duodenal biopsies may then be performed for purposes of differential diagnosis.
3. IgA deficiency is an infrequent but important explanation for why patients with celiac disease may be negative on IgA isotype testing despite strong suspicion. Measuring total IgA levels, IgG deamidated gliadin antibody tests, and TG2-IgG testing in that circumstance is recommended.
4. IgG isotype testing for TG2 antibody is not specific in the absence of IgA deficiency.
5. In patients found to have celiac disease first by intestinal biopsies, celiac-specific serology should be undertaken as a confirmatory test before initiation of a gluten-free diet.
6. In patients in whom celiac disease is strongly suspected in the face of negative biopsies, TG2-IgA should still be performed and, if positive, repeat biopsies might be considered either at that time or sometime in the future.
7. Reduction or avoidance of gluten before diagnostic testing is discouraged, as it may reduce the sensitivity of both serology and biopsy testing.
8. When patients have already started on a gluten-free diet before diagnosis, we suggest that the patient go back on a normal diet with three slices of wheat bread daily preferably for 1 to 3 months before repeat determination of TG2-IgA.
9. Determination of HLA-DQ2/DQ8 has a limited role in the diagnosis of celiac disease. Its value is largely related to its negative predictive value to rule out celiac disease in patients who are seronegative in the face of histologic changes, in patients who did not have serologic confirmation at the time of diagnosis, and in those patients with a historic diagnosis of celiac disease; especially as very young children before the introduction of celiac-specific serology.