1. Lean NAFLD should be diagnosed in individuals with NAFLD and body mass index <25 kg/m2 (non-Asian race) or body mass index <23 kg/m2 (Asian race).
2. Lean individuals with NAFLD should be evaluated routinely for comorbid conditions, such as type 2 diabetes mellitus, dyslipidemia and hypertension.
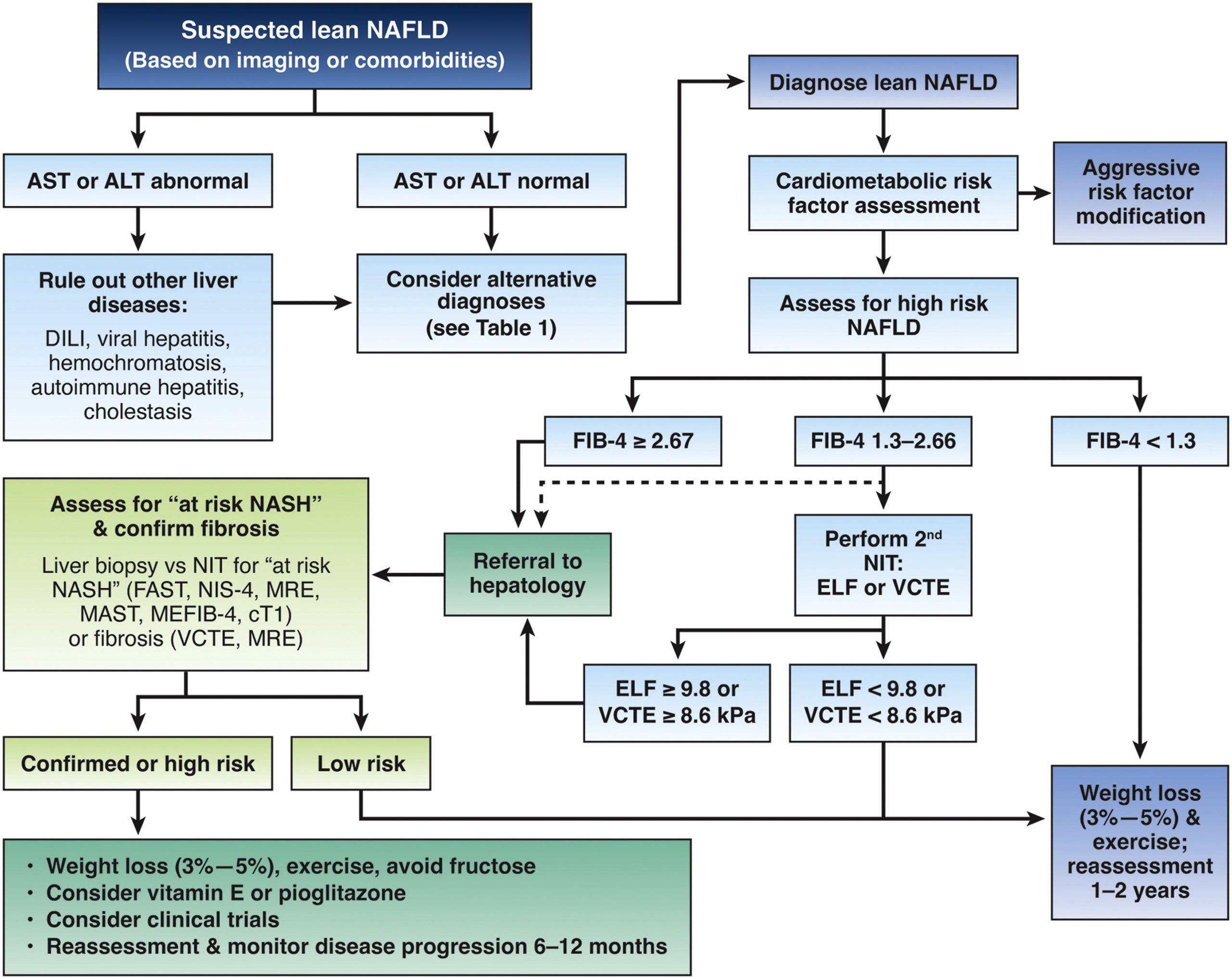
3. Lean individuals with NAFLD should be risk stratified for hepatic fibrosis to identify those with advanced fibrosis or cirrhosis.
4. Lean individuals in the general population should not undergo routine screening for NAFLD; however, screening should be considered for individuals older than 40 years with type 2 diabetes mellitus.
5. NAFLD should be considered in lean individuals with metabolic diseases (such as type 2 diabetes mellitus, dyslipidemia and hypertension), elevated liver biochemical tests or incidentally noted hepatic steatosis.
6. Clinicians should query patients routinely regarding alcohol consumption patterns in all patients with lean NAFLD.
7. In patients with lean NAFLD, other causes of liver disease should be ruled out, including other causes of fatty liver, such as HIV, lipodystrophy, lysosomal acid lipase deficiency, familial hypobetalipoproteinemia and medication-induced hepatic steatosis (methotrexate, amiodarone, tamoxifen and steroids).
8. Current evidence is inadequate to support routine testing for genetic variants in patients with lean NAFLD.
9. Liver biopsy, as the reference standard, should be considered if there is uncertainty regarding contributing causes of liver injury and/or the stage of liver fibrosis.
10. Serum indices (NAFLD fibrosis score and Fibrosis-4 score) and imaging techniques (transient elastography and magnetic resonance elastography) may be used as alternatives to liver biopsy for fibrosis staging and patient follow-up. These tests can be performed at the time of diagnosis and repeated at intervals of 6 months to 2 years, depending on fibrosis stage and the patient’s response to intervention.
11. If noninvasive tests (eg, Fibrosis-4 and NAFLD fibrosis score) are indeterminate, a second noninvasive test (eg, transient elastography or magnetic resonance elastography) should be performed to confirm the stage and prognosis of NAFLD.
12. In lean patients with NAFLD, lifestyle intervention, including exercise, diet modification and avoidance of fructose- and sugar-sweetened drinks, to target a modest weight loss of 3%–5% is suggested.
13. Administration of vitamin E may be considered in lean persons with biopsy-confirmed nonalcoholic steatohepatitis, but without type 2 diabetes mellitus or cirrhosis. Oral pioglitazone 30 mg daily may be considered in lean persons with biopsy-confirmed nonalcoholic steatohepatitis without cirrhosis.
14. The therapeutic role of glucagon-like peptide-1 agonists and sodium-glucose cotransporter-2 inhibitors in the management of lean NAFLD is not fully defined and requires further investigation.
15. Hepatocellular carcinoma surveillance with abdominal ultrasound with or without serum α-fetoprotein twice per year is suggested in patients with lean NAFLD and clinical markers compatible with liver cirrhosis.