1. Gastroenterologists should be aware of potential extraesophageal manifestations of gastroesophageal reflux disease (GERD) and should inquire about such disorders including laryngitis, chronic cough, asthma and dental erosions in GERD patients to determine whether GERD may be a contributing factor to these conditions.
2. Development of a multidisciplinary approach to extraesophageal (EER) manifestations is an important consideration because the conditions are often multifactorial, requiring input from non-gastroenterology specialties. Results from diagnostic testing (i.e., bronchoscopy, thoracic imaging, laryngoscopy, etc.) from non-GI disciplines should be taken into consideration when gastroesophageal reflux (GER) is considered as a cause for extraesophageal symptoms.
3. Currently, there is no single diagnostic tool that can conclusively identify GER as the cause of EER symptoms. Determination of the contribution of GER to EER symptoms should be based on the global clinical impression derived from patients’ symptoms, response to GER therapy, and results of endoscopy and reflux testing.
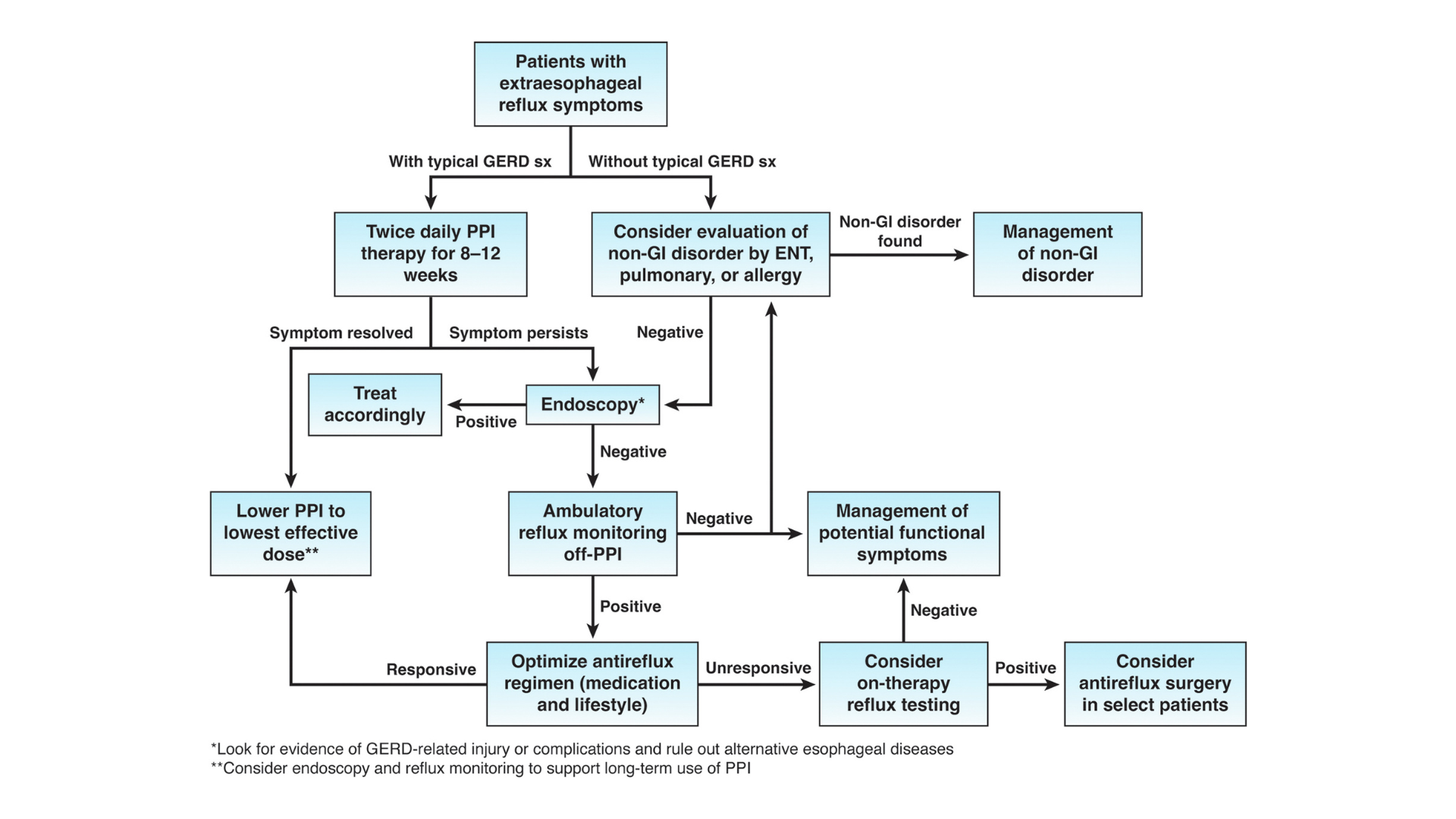
4. Consideration should be given toward diagnostic testing for reflux before initiation of proton pump inhibitor (PPI) therapy in patients with potential extraesophageal manifestations of GERD, but without typical GERD symptoms. Initial single-dose PPI trial, titrating up to twice daily in those with typical GERD symptoms, is reasonable.
5. Symptom improvement of EER manifestations while on PPI therapy may result from mechanisms of action other than acid suppression and should not be regarded as confirmation for GERD.
6. In patients with suspected extraesophageal manifestation of GERD who have failed one trial (up to 12 weeks) of PPI therapy, one should consider objective testing for pathologic GER, because additional trials of different PPIs are low yield.
7. Initial testing to evaluate for reflux should be tailored to patients’ clinical presentation and can include upper endoscopy and ambulatory reflux monitoring studies of acid suppressive therapy.
8. Testing can be considered for those with an established objective diagnosis of GERD who do not respond to high doses of acid suppression. Testing can include pH-impedance monitoring while on acid suppression to evaluate the role of ongoing acid or non-acid reflux.
9. Alternative treatment methods to acid suppressive therapy (e.g., lifestyle modifications, alginate-containing antacids, external upper esophageal sphincter compression device, cognitive-behavioral therapy, neuromodulators) may serve a role in management of EER symptoms.
10. Shared decision-making should be performed before referral for anti-reflux surgery for EER when the patient has clear, objectively defined evidence of GERD. However, a lack of response to PPI therapy predicts lack of response to anti-reflux surgery and should be incorporated into the decision process.