1. Atrophic gastritis is defined as the loss of gastric glands, with or without metaplasia, in the setting of chronic inflammation mainly due to Helicobacter pylori infection or autoimmunity. Regardless of the etiology, the diagnosis of atrophic gastritis should be confirmed by histopathology.
2. Providers should be aware that the presence of intestinal metaplasia on gastric histology almost invariably implies the diagnosis of atrophic gastritis. There should be a coordinated effort between gastroenterologists and pathologists to improve the consistency of documenting the extent and severity of atrophic gastritis, particularly if marked atrophy is present.
3. Providers should recognize typical endoscopic features of atrophic gastritis, which include pale appearance of gastric mucosa, increased visibility of vasculature due to thinning of the gastric mucosa, and loss of gastric folds, and, if with concomitant intestinal metaplasia, light blue crests and white opaque fields. Because these mucosal changes are often subtle, techniques to optimize evaluation of the gastric mucosa should be performed.
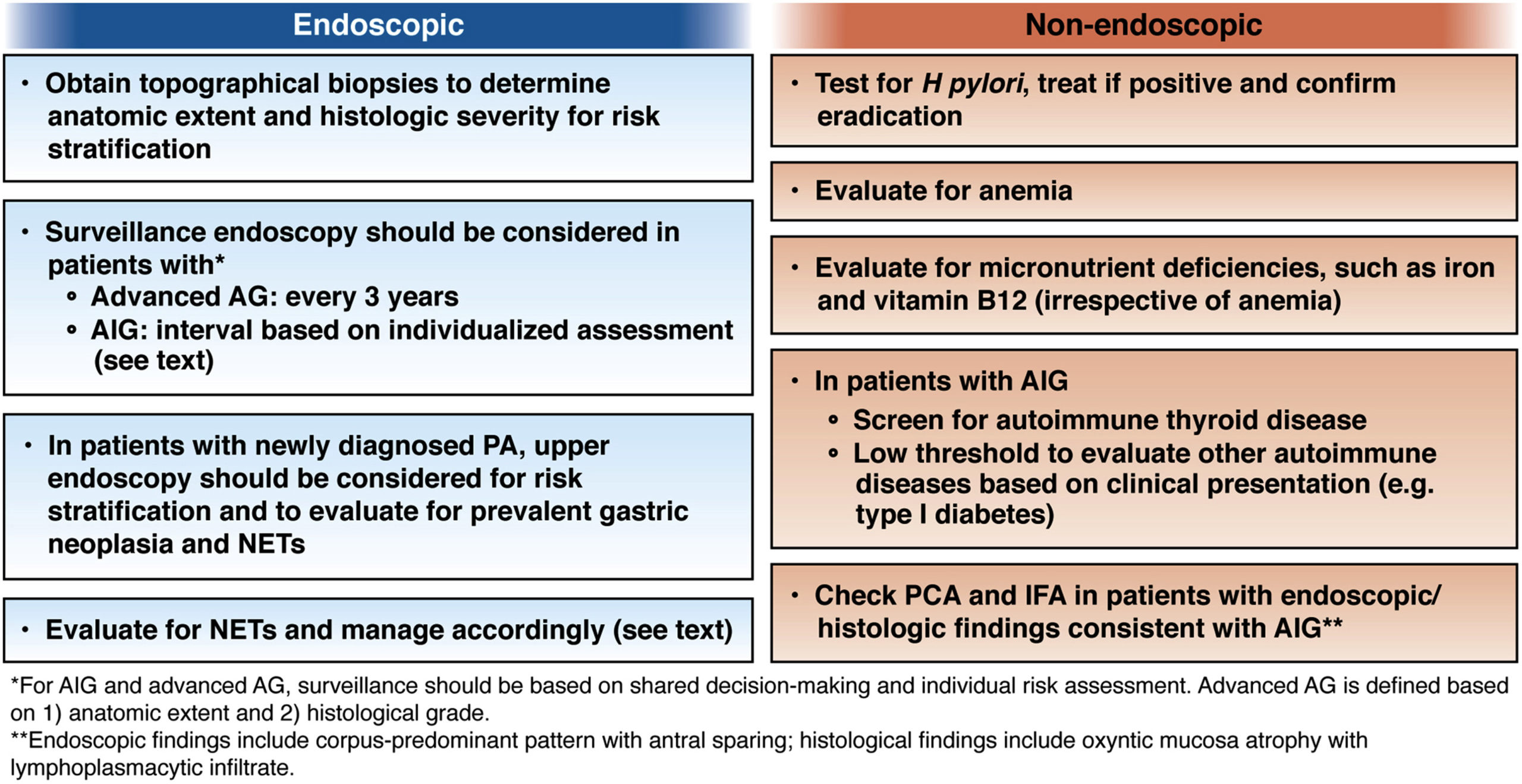
4. When endoscopic features of atrophic gastritis are present, providers should assess the extent endoscopically. Providers should obtain biopsies from the suspected atrophic/metaplastic areas for histopathological confirmation and risk stratification; at a minimum, biopsies from the body and antrum/incisura should be obtained and placed in separately labeled jars. Targeted biopsies should additionally be obtained from any other mucosal abnormalities.
5. In patients with histology compatible with autoimmune gastritis, providers should consider checking antiparietal cell antibodies and anti-intrinsic factor antibodies to assist with the diagnosis. Providers should also evaluate for anemia due to vitamin B-12 and iron deficiencies.
6. All individuals with atrophic gastritis should be assessed for H pylori infection. If positive, treatment of H pylori should be administered and successful eradication should be confirmed using nonserological testing modalities.
7. The optimal endoscopic surveillance interval for patients with atrophic gastritis is not well-defined and should be decided based on individual risk assessment and shared decision making. A surveillance endoscopy every 3 years should be considered in individuals with advanced atrophic gastritis, defined based on anatomic extent and histologic grade.
8. The optimal surveillance interval for individuals with autoimmune gastritis is unclear. Interval endoscopic surveillance should be considered based on individualized assessment and shared decision making.
9. Providers should recognize pernicious anemia as a late-stage manifestation of autoimmune gastritis that is characterized by vitamin B-12 deficiency and macrocytic anemia. Patients with a new diagnosis of pernicious anemia who have not had a recent endoscopy should undergo endoscopy with topographical biopsies to confirm corpus-predominant atrophic gastritis for risk stratification and to rule out prevalent gastric neoplasia, including neuroendocrine tumors.
10. Individuals with autoimmune gastritis should be screened for type 1 gastric neuroendocrine tumors with upper endoscopy. Small neuroendocrine tumors should be removed endoscopically, followed by surveillance endoscopy every 1–2 years, depending on the burden of neuroendocrine tumors.
11. Providers should evaluate for iron and vitamin B-12 deficiencies in patients with atrophic gastritis irrespective of etiology, especially if corpus-predominant. Likewise, in patients with unexplained iron or vitamin B-12 deficiency, atrophic gastritis should be considered in the differential diagnosis and appropriate diagnostic evaluation pursued.
12. In patients with autoimmune gastritis, providers should recognize that concomitant autoimmune disorders, particularly autoimmune thyroid disease, are common. Screening for autoimmune thyroid disease should be performed.