AGA has released two new Clinical Practice Updates (CPUs) in the May issues of Gastroenterology and Clinical Gastroenterology and Hepatology (CGH) providing best practice advice covering the role of diet in irritable bowel syndrome (IBS) treatment and personalized therapeutic approaches for patients experiencing gastroesophageal reflux disease (GERD) symptoms.
DIET IN IRRITABLE BOWEL SYNDROME
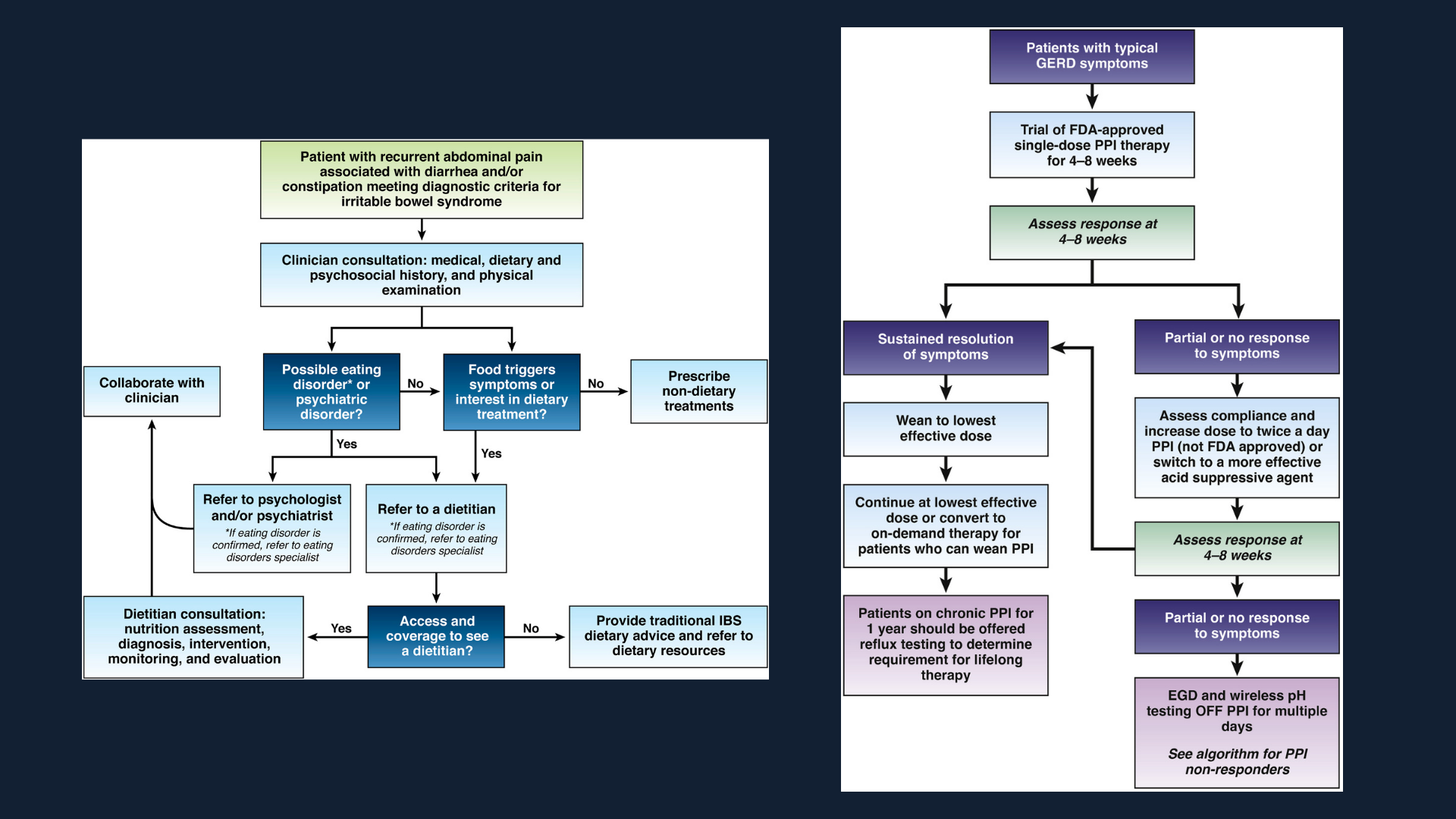
Publishing in Gastroenterology, the authors provide guidance to identify the appropriate dietary treatments for IBS patients such as the low-FODMAP diet and other elimination diets along with the importance of partnering with a registered diet nutritionist. Key advice includes:
- Patients with IBS who are poor candidates for restrictive diet interventions include those consuming few culprit foods, those at risk for malnutrition, those who are food insecure and those with an eating disorder or uncontrolled psychiatric disorder.
- Soluble fiber is efficacious in treating global symptoms of IBS.
- The low-FODMAP diet is currently the most evidence-based diet intervention for IBS.
- Although observational studies found that most patients with IBS improve with a gluten-free diet, randomized controlled trials have yielded mixed results.
PERSONALIZED GERD MANAGEMENT
Publishing in CGH, our experts provide best practices to help you personalize your diagnosis and therapeutic approach for patients experiencing GERD symptoms. This CPU also offers guidance on the importance of educating your patients on GERD pathophysiology, lifestyle modifications and shared decision-making. Key advice includes:
- Clinicians should emphasize safety of proton pump inhibitors (PPIs) for the treatment of GERD.
- Clinicians should provide patients presenting with troublesome heartburn, regurgitation, and/or non-cardiac chest pain without alarm symptoms a 4- to 8-week trial of single-dose PPI therapy. With inadequate response, dosing can be increased to twice a day or switched to a more effective acid suppressive agent once a day. When there is adequate response, PPI should be tapered to the lowest effective dose.
- If PPI therapy is continued in a patient with unproven GERD, clinicians should evaluate the appropriateness and dosing within 12 months after initiation, and offer endoscopy with prolonged wireless reflux monitoring off PPI therapy to establish appropriateness of long-term PPI therapy.
- In patients with proven GERD, laparoscopic fundoplication and magnetic sphincter augmentation are effective surgical options, and transoral incisionless fundoplication is an effective endoscopic option in carefully selected patients.
- Candidacy for invasive anti-reflux procedures includes confirmatory evidence of pathologic GERD, exclusion of achalasia and assessment of esophageal peristaltic function.