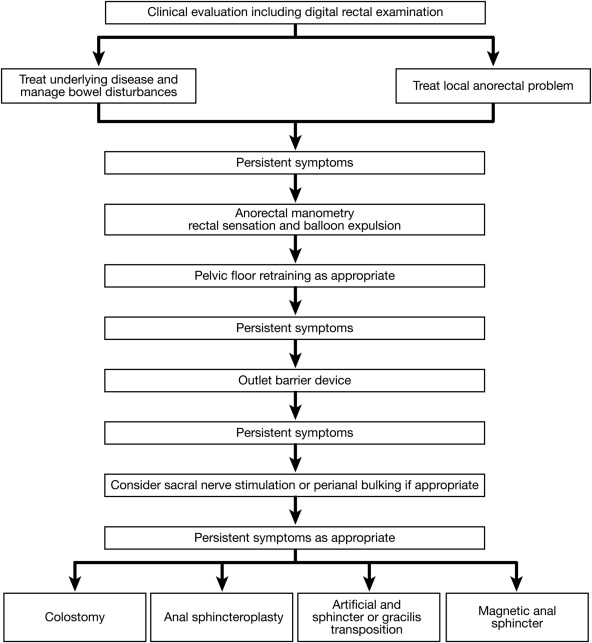
1. A stepwise approach should be followed for management of fecal incontinence (FI). Conservative therapies (diet, fluids, techniques to improve evacuation, a bowel training program, management of diarrhea and constipation with diet and medications if necessary) will benefit approximately 25% of patients and should be tried first.
2. Pelvic floor retraining with biofeedback therapy is recommended for patients with FI who do not respond to the conservative measures indicated above.
3. Perianal bulking agents such as intra-anal injection of dextranomer may be considered when conservative measures and biofeedback therapy fail.
4. Sacral nerve stimulation should be considered for patients with moderate or severe FI in whom symptoms have not responded after a 3-month or longer trial of conservative measures and biofeedback therapy and who do not have contraindications to these procedures.
5. Until further evidence is available, percutaneous tibial nerve stimulation should not be used for managing FI in clinical practice.
6. Barrier devices should be offered to patients who have failed conservative or surgical therapy, or in those who have failed conservative therapy who do not want or are not eligible for more invasive interventions.
7. Anal sphincter repair (sphincteroplasty) should be considered in postpartum women with FI and in patients with recent sphincter injuries. In patients who present later with symptoms of FI unresponsive to conservative and biofeedback therapy and evidence of sphincter damage, sphincteroplasty may be considered when perianal bulking injection and sacral nerve stimulation are not available or have proven unsuccessful.
8. The artificial anal sphincter, dynamic graciloplasty, may be considered for patients with medically refractory severe FI who have failed treatment or are not candidates for barrier devices, sacral nerve stimulation, perianal bulking injection, sphincteroplasty and a colostomy.
9. Major anatomic defects (eg, rectovaginal fistula, full-thickness rectal prolapse, fistula in ano, or cloaca-like deformity) should be rectified with surgery.
10. A colostomy should be considered in patients with severe FI who have failed conservative treatment and have failed or are not candidates for barrier devices, minimally invasive surgical interventions, and sphincteroplasty.
11. A magnetic anal sphincter device may be considered for patients with medically refractory severe FI who have failed or are not candidates for barrier devices, perianal bulking injection, sacral nerve stimulation, sphincteroplasty, or a colostomy. Data regarding efficacy are limited and 40% of patients had moderate or severe complications.
12. For defecatory disorders, biofeedback therapy is the treatment of choice.
13. Based on limited evidence, sacral nerve stimulation should not be used for managing defecatory disorders in clinical practice.
14. Anterograde colonic enemas are not effective in the long term for management of defecatory disorders.
15. The stapled transanal rectal resection and related procedures should not be routinely performed for correction of structural abnormalities in patients with defecatory disorders.