AGA’s latest Clinical Practice Update, authored by Drs. Jordan Axelrad, Jana Hashash and Steven Itzkowitz, and published in Clinical Gastroenterology and Hepatology, addresses how best to approach the risk of malignancy as well as how to manage active cancer in patients with IBD.
Quick watch: Authors Drs. Jordan Axelrad and Steven Itzkowitz discuss which cancers have been associated with IBD and its medical therapies as well as how to manage IBD if a patient develops an active cancer.
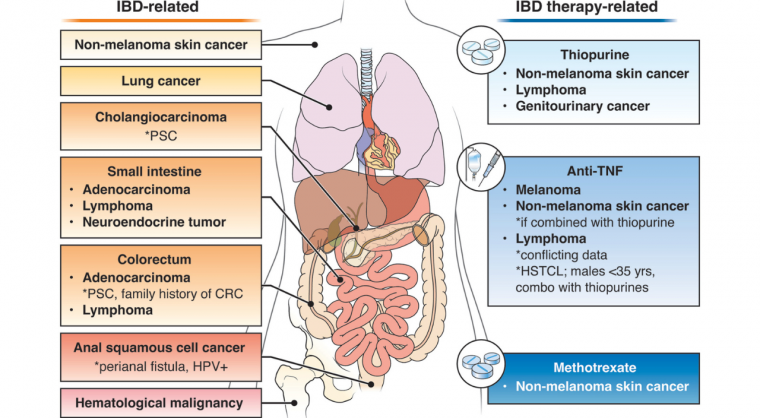
Patients with IBD are at risk for the following cancers:
CRC is one of the most common malignancies in patients with IBD and is a direct consequence of chronic colonic inflammation.
Other risk factors include: long disease duration, increased colonic involvement, family history of CRC and having primary sclerosing cholangitis.
Patients with Crohn’s disease and small bowel inflammation are at an increased risk for small bowel adenocarcinoma and neuroendocrine tumors.
Additional risk factors include: tobacco use, male sex, childhood onset Crohn’s disease, long-standing small bowel inflammation, penetrating or stricturing disease and prior small bowel resection.
Intestinal lymphoma is estimated to occur at a two- to three-fold increased in individuals with IBD compared with the general population. These cancers occur more often in males, those with ongoing intestinal inflammation and in patients who have had Crohn’s disease for more than eight years.
The absolute risk of anal cancer among patients with Crohn’s disease remains low, but higher than the general population. Additional risk factors include HPV and long-standing perianal fistualizing disease.
Cholangiocarcinoma is four times more likely to occur in patients with IBD compared with patients without IBD. Patients with primary sclerosing cholangitis are at the highest risk.
Patients with IBD are also at an increased risk for nonmelanoma skin cancers, hematologic malignancy and lung cancer.
Looking at cancer risk associated with IBD therapies
There is an increased risk of non-melanoma skin cancer at an almost two-fold increase.
Non-intestinal lymphoma is also an associated risk of thiopurine use as is genitourinary cancers.
Data is limited, but studies show a small increased risk of non-melanoma skin cancer.
The data linking anti-TNF therapy with lymphoma and melanoma are conflicting. However, there is an increased risk of lymphoma when anti-TNF agents are combined with thiopurines.
In IBD patients, there has been no data so far to suggest an increased risk of malignancy. However, clinical trial data for patients with rheumatoid arthritis on JAK inhibitors showed an increased risk of malignancy, particularly non-melanoma skin cancer, lung cancer and lymphoma.
Current evidence does not show an increased risk of malignancy in patients with IBD treated with vedolizumab, ustekinumab, risankizumab, mirikizumab, ozanimod and etrasimod, although, long-term data are lacking.
Read the full AGA Clinical Practice Update on Management of Inflammatory Bowel Disease in Patients With Malignancy: Commentary, published in the July issue of Clinical Gastroenterology and Hepatology.