Through the end of the year, we’re bringing back some of the best articles from the AGA Journals blog, Digest This. Learn more about serrated colorectal polyps in this article from September 2019.
Serrated polyps comprise hyperplastic polyps, sessile serrated lesions (SSLs) and traditional serrated adenomas (TSAs). Approximately 25 percent of sporadic colorectal cancers (CRCs) arise from serrated precursor lesions, but there is confusion regarding their terminology, classification, and risk. A review article by Seth D. Crockett and Iris D. Nagtegaal in the October 2019 issue of Gastroenterology clarifies these issues and explains why SSLs and proximal hyperplastic polyps require special attention.
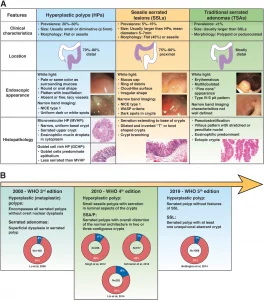
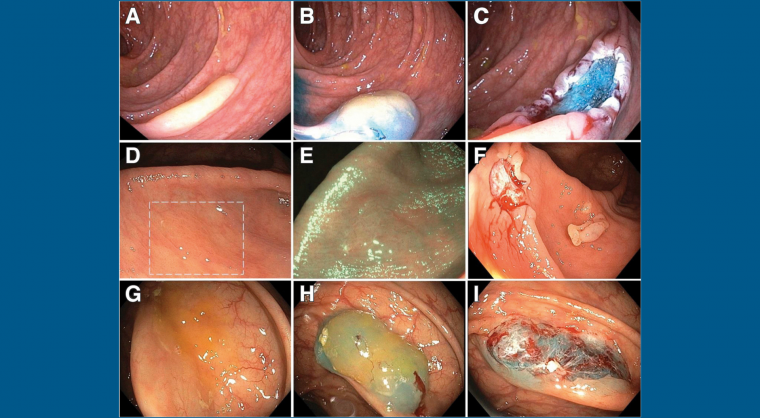
Clinical, endoscopic, and histologic characteristics of the different serrated polyps.
Hyperplastic polyps account for approximately 75% all serrated polyps, whereas SSLs (previously called sessile serrated adenomas or sessile serrated polyps) account for approximately 25%. SSLs are characterized by a larger size, location in the proximal colon, and endoscopic appearance, which is distinct from that of hyperplastic polyps (see figure). TSAs are the least-common type of serrated polyp — they are typically polypoid lesions found in the distal colorectum. SSLs and TSAs are each considered as precursors to CRC.
Crockett and Nagtegaal review what we have learned about serrated lesions, criteria for management of serrated neoplasias, molecular and epidemiologic features, methods of detection, and surveillance recommendations for patients with serrated polyps. In 2019, the World Health Organization published their latest definitions for SSLs and hyperplastic polyps and changes in prevalence of diagnostic categories (see figure part B).
The authors review the steps in the serrated pathway, molecular changes during progression of polyps, and features of colorectal tumors that arise from serrated lesions. For example, the authors state that colorectal tumors with BRAF mutations (3-8 percent of CRCs) are likely to be derived from SSLs. They discuss serrated polyposis syndrome, in which patients develop multiple serrated polyps throughout the colorectum and have an increased risk of CRC, and genetic alterations associated with development of SSAs.
There is a large amount of geographic variation in the prevalence of serrated polyps, with high prevalence in the United Kingdom, New Zealand and the United States, and low prevalence in Singapore and Japan. In contrast to conventional adenomas, older age and male sex are not strong risk factors for SSLs. Although patients younger than 50 years have a lower risk of SSLs than patients older than 50 years, risk does not appear to increase substantially with age beyond 50 years. Men and women have similar risks for SSL. Smoking, body mass index, and alcohol intake can increase risk for serrated polyps (smoking increases risk for SSLs in particular).
Crockett and Nagtegaal review the best strategies for detection and resection of serrated polyps. Patients with patients with SSLs have a 2- to 4-fold increased risk of synchronous advanced neoplasia, metachronous high-risk adenomas, and CRC of the proximal colon. They discuss surveillance guidelines for patients who have serrated polyps removed during screening or surveillance colonoscopies, and differences in recommendations among global regions.
The authors conclude that many controversies surround serrated neoplasias, and that additional studies are needed to refine recommendations. Identification of SSLs based on pathology features, and in particular to differentiate hyperplastic polys from SSLs, can be a challenge and there are differences in surveillance guidelines for patients with serrated lesions. Efforts are needed, worldwide, to optimize detection, resection and classification of serrated polyps and lesions, and to determine the most appropriate surveillance practices for the patients who have them.

Kristine Novak, MD
Dr. Novak is a science writer and editor based in San Francisco. She has extensive experience covering gastroenterology, hepatology, immunology, oncology, clinical and biotechnology research discoveries.