AGA Campaign to #StopUHC
Home > Advocacy & Policy > Policies Affecting GI > AGA campaign to block UnitedHealthcare GI prior auth policy
AGA campaign to block UHC's GI prior auth policy
AGA continues to demand that UnitedHealthcare (UHC) provide details, transparency and policies that put patients first.
AGA priority: Protecting GI patients and practices from prior auth policies that don’t put patients first.
Here's how we're fighting for GI
AGA will not let UHC quietly role out a prior authorization program that will impact millions of patients nationwide.
-
We're raising public awareness
We're speaking with the media on a daily basis and working with our members to author op-eds explaining this ill-informed policy.
-
We're engaging legislators
We're working with our partners on the Hill to write UnitedHealthcare and demand transparency. Rep. Donald Payne Jr. also delivered a floor speech denouncing this policy.
-
We're questioning UHC
AGA Past President Dr. Barbara Jung wrote UHC expressing gastroenterologists’ worries around three key areas of concern: transparency, practice burden, and lack of details on the impending gold card program.
-
We're bringing the fight to social media
Help us by tweeting with the hashtag #StopUHC.
Latest news

Dr. Maria Abreu
Q&A: AGA snubs UHC’s choice to ‘forgo transparency’ in Gold Card program for GI endoscopy — Healio Gastroenterology, Aug. 23, 2024

Dr. Maria Abreu
American Gastroenterological Association slams UnitedHealthcare gold card program — Becker’s GI & Endoscopy, Aug. 8, 2024

Dr. Andrea Shin
Dr. Joseph Feuerstein
- Ongoing #StopUHC campaign calls on UHC to rethink looming program on GI procedures — Healio, June 26, 2024
- Colorectal cancer is the nation’s 2nd deadliest. Why is my insurer making it harder to prevent? — Minnesota Reformer, March 28, 2024 (authored by patient advocate Kimberly Hooks)
- The ‘Gold Card’ Shuffle — KFF Health News, Feb. 29, 2024 (authored by Dr. Barbara Jung)
- Why Are We Letting Insurers Dictate Patient Care? — MedPage Today, Jan. 30, 2024 (authored by Drs. Barbara Jung and Deborah Dyett Desir)
- Digestive Health Is Women’s Health. Insurance Barriers Block Access to Both. — The Well News, Nov. 3, 2023 (authored by Dr. Shazia Siddique)
- UnitedHealthcare’s Advance Notification program is getting in the way of patient care — Fierce Healthcare, Nov. 3, 2023 (authored by Dr. Jessica Korman)
- Congress: Remove insurance barriers to care — Orlando Sentinel, Nov. 2, 2023 (authored by Karen Mancera Azamar)
- For Shame, UnitedHealthcare — KFF Health News, Sep. 28, 2023 (authored by Dr. Lawrence Kim)
- UnitedHealthcare policies undermine gastrointestinal care — South Florida Sun Sentinel, Aug. 8, 2023 (authored by Dr. Maria Abreu)
- Insurer tactics to delay care pushes health equity further away — Capitol Weekly, July 31, 2023 (authored by Dr. Fola May)
- Insurers such as UnitedHealthcare should not make it harder to get a colonoscopy — The Tennessean, July 26, 2023 (authored by Rep. Mark Green)
- Insurance companies putting up too many barriers — Daily Herald, July 25, 2023 (authored by Dr. Joseph Losurdo)
- Prior authorization, by any other name, threatens Washingtonians’ health — The Olympian (authored by Dr. Barbara Jung), July 19, 2023
- UHC should reverse course on prior authorization policy — Dallas Morning News (authored by Dr. Rajeev Jain), July 13, 2023
- UnitedHealthcare shifts colonoscopy requirements from controversial ‘prior authorization’ to ‘advance notification’ — CNN, June 1, 2023
- UnitedHealthcare nixes prior authorization rule, but docs aren’t happy about what’s replaced it — Fierce Healthcare, June 1, 2023
- UnitedHealth backs off contentious prior authorization plan — Axios, June 1, 2023
- UnitedHealth Ditches Controversial Prior Authorization for GI Procedures for ‘Advance Notification Process’— Managed Healthcare Executive, June 1, 2023
- GI Docs Reject UHC Plan To Replace Prior Auth With Advanced Notification — Inside Health Policy, May 31, 2023
- How UHC’s new prior authorization policy for colonoscopies could make patients wait — Fierce Healthcare (authored by Dr. Barbara Jung), May 26, 2023
- Doctors and patients are worried this large health insurer’s new policy will delay care — USA Today, May 24, 2023
- Gastro Docs Demand United Reverse Prior Auth Changes Set For June 1 — Inside Health Policy, May 23, 2023
- UnitedHealthcare draws fire from docs over new prior authorization policy for colonoscopies — Fierce Healthcare, May 16, 2023
- UnitedHealthcare will soon implement a controversial prior authorization policy for surveillance and diagnostic colonoscopies — Forbes, May 16, 2023
- ‘Stunning’ change to United’s colonoscopy coverage roils physicians and patients — STAT News, May 15, 2023
Background
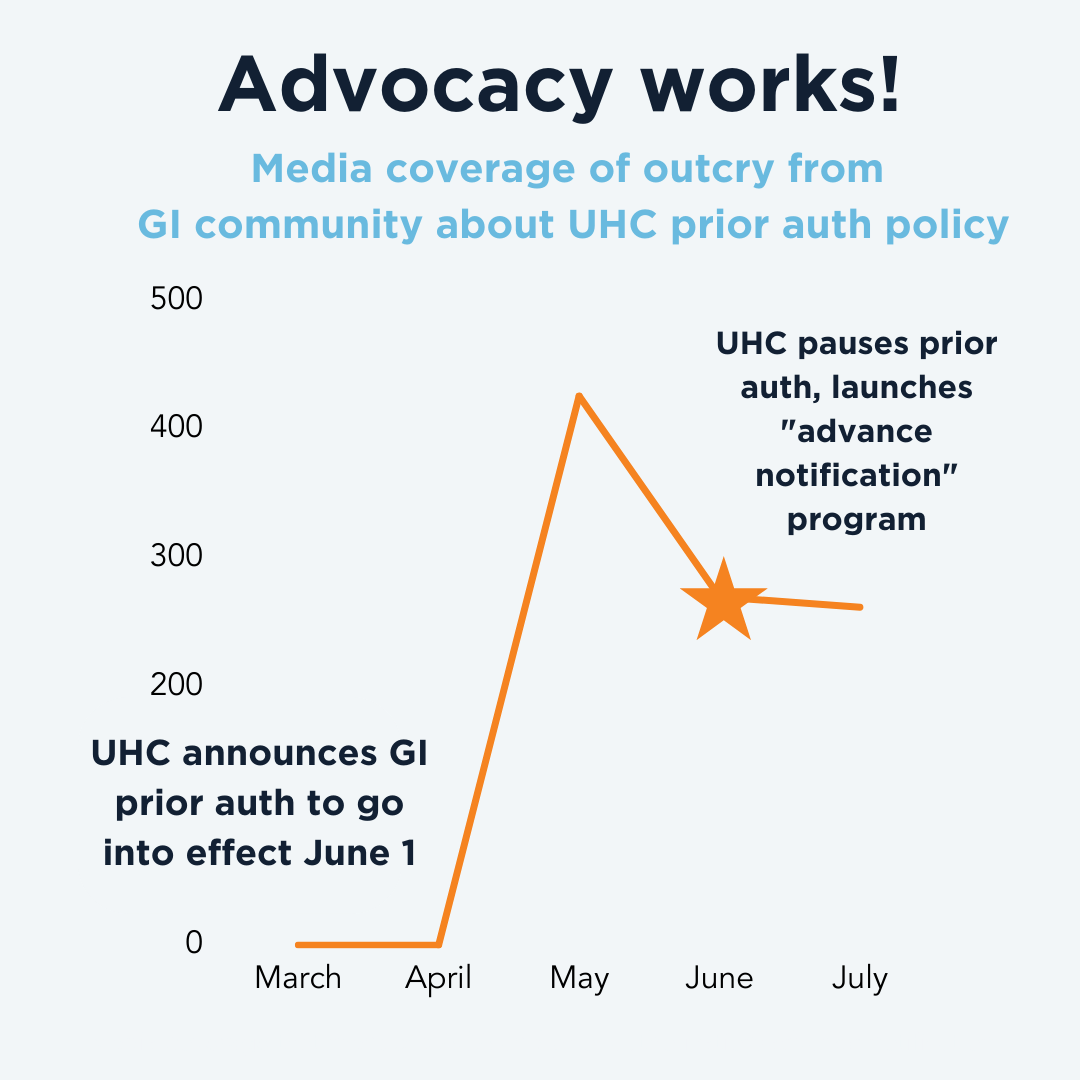
After weeks of protest from AGA and the GI community, UnitedHealthcare shelved the prior authorization policy for GI endoscopy planned to go into effect June 1, 2023, but replaced it with a nebulous Advance Notification Program.
This program requires you to provide even more data on top of the current burdensome paperwork requirements. It is a temporary patch – patients will not be denied care immediately, but this program laid the groundwork for a sweeping prior authorization program.
On Aug. 1, 2024, UHC quietly announced to media a new “Gold Card” prior authorization program, set to launch Oct. 1, 2024. At this time, AGA does not expect the UHC Gold Card program will have major effects for GI practices. However, UHC provided scant details with their program announcement and has not provided useful information in response to AGA inquiries. If you receive information from UHC representatives, please let us know. We’re ready to advocate for GIs and our patients.
- UHC’s Gold Card program: Status quo — Sept. 4, 2024
- Here we go again: UHC announces “gold card” program, AGA demands details — Aug. 9, 2024
- UHC’s promise to impose prior authorization for virtually all colonoscopies and endoscopies in “early 2024” puts critical care in limbo for its 27 million commercial beneficiaries — Dec. 20, 2023
- AGA, patient groups remain deeply troubled by UHC’s barriers to GI care — Dec. 12, 2023
- GI patients and physicians urge Congress to fight back against out-of-control prior authorization — Sept. 21, 2023
- One month after UnitedHealthcare’s “advance notification” program began, confusion still reigns for America’s GI doctors — July 6, 2023
- Despite last minute change, UnitedHealthcare’s policy for virtually all colonoscopies and endoscopies lays groundwork for delays, disruptions, and denials of life-saving services — June 1, 2023
- GI society statement: UHC offers to trade GI prior auth for a poorly defined alternative — May 26, 2023
- AGA doubles down on prior auth fight with UHC — May 10, 2023
- TIME IS RUNNING OUT: Patients, Physicians Brace for Anticipated Delays, Denials by UnitedHealthcare for Endoscopies Starting 6/1 — May 1, 2023
Bottom line: Patients should have timely access to the care their health care providers deem medically necessary.
For more information
Contact the AGA Government Affairs team: [email protected]. Media: contact Rebecca Reid at [email protected] or 410-212-3843.











